Overview
Arteriosclerosis and atherosclerosis are often used interchangeably, but they are not the same condition.
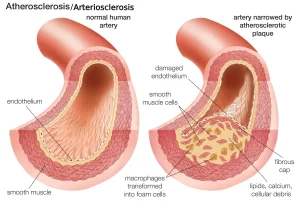
Arteriosclerosis is a general term that refers to the thickening and stiffening of arteries. Arteries are blood vessels that carry oxygen- and nutrient-rich blood from the heart to the rest of the body. Healthy arteries are flexible and elastic, allowing blood to flow easily. With arteriosclerosis, the artery walls lose this flexibility and become stiff, a process commonly known as hardening of the arteries.
Atherosclerosis is a specific type of arteriosclerosis. In this condition, fats, cholesterol and other substances build up in and on the artery walls. This buildup is known as plaque. Plaque can narrow the arteries and reduce blood flow. In some cases, plaque can rupture, which may lead to the formation of a blood clot.
Although atherosclerosis is often associated with heart disease, it can affect arteries anywhere in the body. With proper treatment and healthy lifestyle changes, atherosclerosis can be managed and its progression slowed.
Symptoms
Mild atherosclerosis usually does not cause noticeable symptoms.
Symptoms typically appear only when an artery becomes significantly narrowed or completely blocked, reducing blood flow to organs and tissues. In some cases, a blood clot may suddenly block blood flow, or break loose and cause a medical emergency such as a heart attack or stroke.
Symptoms vary depending on which arteries are affected.
If the arteries supplying the heart are involved, symptoms may include chest pain or pressure, known as angina.
If arteries leading to the brain are affected, symptoms may include sudden numbness or weakness in the arms or legs, difficulty speaking, slurred speech, temporary or sudden loss of vision in one eye, or drooping of facial muscles. These symptoms may indicate a transient ischemic attack (TIA), which can lead to a stroke if left untreated.
If arteries in the arms or legs are affected, symptoms may include pain in the legs while walking, known as claudication. This is a sign of peripheral artery disease. Lower blood pressure may also be present in the affected limb.
If the arteries supplying the kidneys are narrowed, atherosclerosis may lead to high blood pressure or kidney failure.
When to see a doctor
If you believe you may have atherosclerosis, schedule a medical checkup. Early diagnosis and treatment can help prevent the condition from worsening and may reduce the risk of heart attack, stroke or other serious complications.
Seek emergency medical care if you experience chest pain or symptoms suggestive of a TIA or stroke, such as:
-
Sudden numbness or weakness in the arms or legs
-
Difficulty speaking or slurred speech
-
Sudden or temporary loss of vision in one eye
-
Drooping of facial muscles
Causes
Atherosclerosis develops slowly over time and may begin as early as childhood. The exact cause is not fully understood, but it often starts with damage to the inner lining of an artery.
Factors that can damage the artery lining include:
-
High blood pressure
-
High cholesterol
-
High triglycerides, a type of fat in the blood
-
Smoking or other tobacco use
-
Diabetes
-
Insulin resistance
-
Obesity
-
Chronic inflammation from unknown causes or from conditions such as arthritis, lupus, psoriasis or inflammatory bowel disease
Once the artery lining is damaged, blood cells and other substances collect at the site of injury. Over time, fats, cholesterol and other materials accumulate and form plaque within the artery walls. This plaque narrows the arteries and limits blood flow. If plaque ruptures, a blood clot may form and further block blood flow.
Risk factors
Some risk factors for atherosclerosis cannot be changed, including increasing age, a family history of early heart disease or stroke, genetic changes that increase susceptibility to atherosclerosis, and the presence of chronic inflammatory conditions such as lupus, psoriasis or inflammatory bowel disease.
Other risk factors can often be managed or controlled. These include an unhealthy diet, diabetes, high blood pressure, high cholesterol, lack of physical activity, obesity, sleep apnea, and smoking or other tobacco use.
Complications
Complications of atherosclerosis depend on which arteries are affected.
When arteries supplying the heart are involved, coronary artery disease may develop. This can lead to chest pain, heart attack or heart failure.
Atherosclerosis in arteries supplying the brain may cause carotid artery disease, increasing the risk of transient ischemic attack or stroke.
If arteries in the arms or legs are affected, peripheral artery disease may occur. Reduced blood flow can cause pain, poor wound healing, or in rare cases, tissue death known as gangrene.
Atherosclerosis can also weaken artery walls and lead to the formation of an aneurysm, which is a bulge in the artery wall. Most aneurysms do not cause symptoms, but if one ruptures, it can result in life-threatening internal bleeding.
When arteries supplying the kidneys are narrowed, chronic kidney disease may develop. Reduced blood flow prevents the kidneys from receiving enough oxygen-rich blood, impairing their ability to remove waste and excess fluid from the body.
Prevention
The same lifestyle changes used to treat atherosclerosis can also help prevent it and support overall artery health.
Key preventive measures include:
-
Avoiding smoking and all forms of tobacco
-
Eating a nutritious, balanced diet
-
Engaging in regular physical activity
-
Maintaining a healthy body weight
-
Managing blood pressure, blood sugar and cholesterol levels consistently
Advertisement