Overview
Athlete’s foot, also called tinea pedis, is a common fungal skin infection that usually begins between the toes. It develops most often when feet become warm, moist and sweaty, especially after being enclosed in tight-fitting shoes for long periods.
The infection is caused by fungi known as dermatophytes, which thrive in warm and damp environments. Athlete’s foot is contagious and can spread through direct contact with an infected person or through contact with contaminated surfaces such as floors, towels, socks or shoes.
Athlete’s foot is closely related to other fungal infections, including ringworm and jock itch, and the same type of fungus may cause all three conditions. Although antifungal treatments are effective, athlete’s foot often returns, particularly if preventive measures are not followed.
Symptoms
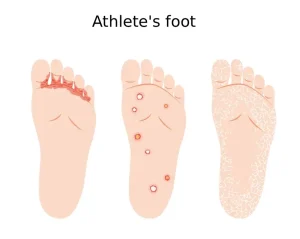
Athlete’s foot can affect one or both feet, and symptoms may vary depending on skin type and the severity of the infection. The condition often causes discomfort that worsens after shoes and socks are removed.
Common symptoms of athlete’s foot include:
-
Scaly, peeling or cracked skin between the toes
-
Itching, especially after removing shoes and socks
-
Inflamed skin that may appear reddish, purplish or grayish depending on skin tone
-
Burning or stinging sensations
-
Blisters
-
Dry, scaly skin on the sole of the foot that may extend up the sides
If symptoms do not improve within two weeks of using over-the-counter antifungal treatments, medical evaluation is recommended. People with diabetes or signs of infection such as swelling, pus or fever should seek medical care promptly.
Causes
Athlete’s foot is caused by dermatophyte fungi, the same group of fungi responsible for ringworm and jock itch. These fungi grow best in warm, humid environments, such as sweaty socks and enclosed shoes.
The infection spreads easily through:
-
Direct skin-to-skin contact with an infected person
-
Contact with contaminated surfaces, including floors, towels, socks and footwear
The fungus can also spread from the feet to other parts of the body, especially if the infected areas are scratched or touched and then other areas are handled without washing.
Risk factors
Certain factors increase the likelihood of developing athlete’s foot by creating conditions that favor fungal growth or exposure.
Risk factors include:
-
Frequently wearing enclosed or tight-fitting footwear
-
Excessive sweating of the feet
-
Sharing shoes, socks, towels or bedding with someone who has a fungal infection
-
Walking barefoot in public places such as locker rooms, showers, saunas, swimming pools or communal bathing areas
Complications
Athlete’s foot can spread to other warm and moist areas of the body if left untreated. The same fungus often causes jock itch, and the infection may spread from the feet to the groin through hands, towels or clothing.
In some cases, athlete’s foot can lead to secondary bacterial infections, particularly if the skin becomes cracked or broken. This risk is higher in people with diabetes or weakened immune systems.
Prevention
Simple hygiene and footwear habits can help prevent athlete’s foot and reduce the risk of spreading the infection.
Preventive measures include:
-
Allowing feet to air out by wearing sandals or open shoes when possible
-
Washing feet daily with warm, soapy water and drying thoroughly, especially between the toes
-
Using medicated or antifungal foot powders if prone to fungal infections
-
Changing socks at least once a day, or more often if feet sweat heavily
-
Choosing moisture-wicking socks to help keep feet dry
-
Alternating shoes daily to allow them to dry completely between uses
-
Wearing protective footwear such as sandals in public showers, pools and locker rooms
-
Avoiding sharing shoes, socks, towels or unwashed bedding with others
Consistent preventive care can help reduce recurrence and limit the spread of athlete’s foot.
Advertisement