Overview
cute Liver Failure: Diagnosis, Tests, and Advanced Treatment Options
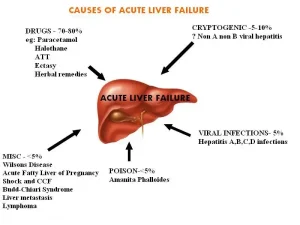
Acute liver failure is a serious and life-threatening condition that requires immediate medical attention. Early diagnosis and treatment can significantly improve outcomes and may even help avoid a liver transplant. Here’s a detailed look at the tests, procedures, and treatments used to diagnose and manage acute liver failure effectively.
Diagnosis of Acute Liver Failure
Doctors use several tests and procedures to identify liver damage and determine the underlying cause of acute liver failure.
• Blood Tests (Liver Function Tests): Blood tests help measure how well your liver is functioning. A prothrombin time test is especially important — it shows how long it takes your blood to clot. In acute liver failure, blood takes longer to clot, indicating liver dysfunction.
• Imaging Tests (Ultrasound, CT & MRI): A liver ultrasound is often the first step to check for liver damage. If more detail is needed, doctors may use abdominal CT scanning or MRI to examine the liver and blood vessels. These imaging tests help detect issues like Budd–Chiari syndrome, blockages, or tumors when ultrasound alone isn’t enough.
• Liver Biopsy: In some cases, a liver biopsy may be required to determine why the liver is failing. Since patients with acute liver failure have a higher risk of bleeding, a transjugular liver biopsy is often used. This involves inserting a thin catheter through a vein in the neck to safely collect a tissue sample.
Treatment Options for Acute Liver Failure
Patients with acute liver failure are usually treated in an intensive care unit—preferably at a hospital equipped to perform a liver transplant if needed. Treatment aims to reverse liver damage, manage complications, and support liver recovery.
• Medications to Reverse Poisoning: Acute liver failure caused by acetaminophen overdose can be treated with acetylcysteine. Certain mushroom or toxin-induced liver failures can also be treated with specific antidotes to reduce liver damage.
• Liver Transplant Surgery: If the liver cannot recover, a liver transplant may be the only treatment option. The damaged liver is removed and replaced with a healthy donor liver, offering the best chance of long-term survival.
• Managing Complications: Medications are used to reduce brain swelling (cerebral edema). Regular tests help detect infections early. Medicines and blood transfusions can prevent or control bleeding. Nutritional supplements are given if the patient cannot eat normally.
Emerging & Future Treatments for Acute Liver Failure
Researchers are continuously working on innovative therapies to reduce the need for a full liver transplant. These experimental treatments may offer new hope in the future:
• Artificial Hepatic Assist Devices: These machines temporarily perform liver functions, similar to dialysis for kidney failure. One promising method is high-volume plasma exchange.
• Hepatocyte Transplantation: This involves transplanting only liver cells rather than the entire organ, which may delay or even prevent the need for a full transplant.
• Auxiliary Liver Transplantation: A small section of the liver is replaced with a matching graft, allowing the natural liver to regenerate without long-term immunosuppressants.
• Xenotransplantation: Using a non-human donor liver (such as a pig liver) is an experimental option being re-explored with modern technology and improved transplant methods.
Advertisement