Overview
Diagnosis
If your symptoms don’t improve with at-home care, it’s important to see a healthcare professional or seek emergency help. Even if symptoms improve, your provider may want to examine you to ensure your asthma is under control, depending on severity.
At a clinic or emergency room, treatment and testing often happen simultaneously. The goal is to improve breathing, assess attack severity, and monitor treatment effectiveness.
Tests to measure lung function
-
Peak flow meter. Measures how quickly you can exhale. Peak flow readings are expressed as a percentage of your personal best.
-
Spirometry. Determines the volume of air your lungs hold and the speed of exhalation, called forced expiratory volume (FEV-1). FEV-1 is compared with normal values to assess airway obstruction.
-
Pulse oximeter. A small device clipped on your finger measures oxygen levels in your blood, indicating how effectively your lungs are delivering oxygen.
-
Nitric oxide measurement. Detects inflammation in the airways by measuring nitric oxide in exhaled breath. This test is rarely used in emergency situations.
Treatment
Management of an asthma attack starts with following your asthma action plan at home. The plan guides when to continue home care, contact your healthcare provider, or seek urgent medical attention.
Yellow zone
The yellow zone indicates moderate symptoms or a peak flow reading between 50% and 79% of your personal best. Your action plan will specify:
-
Quick-relief inhalers. Medicines include:
-
Albuterol (ProAir HFA, Proventil HFA, Ventolin HFA, others)
-
Levalbuterol (Xopenex, Xopenex HFA)
-
-
Dosage instructions. When to repeat doses and when to take an oral corticosteroid for inflammation.
-
Monitoring guidance. Signs to watch for and when to contact your healthcare provider.
Young children or patients who struggle with inhalers may use a nebulizer to inhale the medicine as a mist.
Red zone
Seek emergency care immediately if:
-
Severe shortness of breath occurs
-
Symptoms worsen despite home treatment
-
You remain in the yellow zone after 24 hours
-
Daily activities become difficult
-
Peak flow drops below 50% of your personal best
-
Your healthcare provider advises urgent care
Emergency treatment
In the emergency room, treatment focuses on restoring breathing and oxygenation:
-
Oxygen therapy. Administered through nasal tubes or masks to maintain adequate oxygen levels.
-
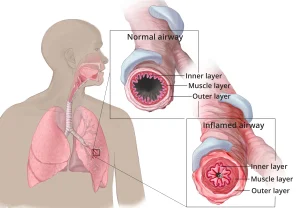
Quick-relief inhalers or nebulizers. Medicines like albuterol or levalbuterol open narrowed airways.
-
Ipratropium (Atrovent HFA). Another inhaled bronchodilator to relax airways.
-
Corticosteroids. Given orally or by injection to reduce inflammation.
-
Mechanical ventilation. For life-threatening attacks, a machine may assist breathing. Intubation may be required in severe cases.
Patients remain under observation until breathing stabilizes.
Follow-up care
After an attack, you will receive instructions on:
-
Daily long-term medications and dosage
-
Quick-relief medication use and timing
-
Scheduling follow-up visits with your regular healthcare provider
-
Recognizing when to seek urgent or emergency care
Advertisement