Overview
Diagnosis
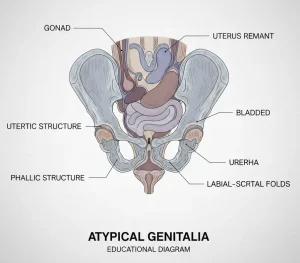
Atypical genitalia is usually diagnosed at birth or shortly after. In rare cases, it may be suspected before birth if blood tests of the unborn baby’s sex differ from ultrasound findings. Healthcare professionals attending the birth may notice atypical genitalia in the newborn.
Determining the Cause
Once atypical genitalia is suspected, doctors aim to identify the underlying cause. Understanding the cause helps guide treatment decisions and sex assignment. Steps include:
Medical history and physical exam
-
Doctors ask about family and medical history.
-
Physical exam checks for testicles and evaluates genital appearance.
Tests may include:
-
Blood tests for hormone levels to check for imbalances.
-
Chromosomal blood tests to determine genetic sex (XX or XY) and identify genetic conditions affecting sex organ development.
-
Ultrasound of the pelvis and abdomen to locate undescended testicles or evaluate internal reproductive structures.
-
X-rays with contrast dye for detailed imaging of pelvic structures.
-
Minimally invasive surgery in some cases to collect tissue samples using small cameras and instruments.
Deciding the Sex
Sex assignment is based on multiple factors:
-
Cause of atypical genitalia
-
Genetic sex
-
Anatomy and potential reproductive function
-
Probable adult gender identity
-
Discussion with parents
Timing of decision can vary. While some families may decide within days, tests should be completed first, and in some cases, the child’s future gender identity may influence later decisions.
Treatment
The goal of treatment is long-term mental health, social well-being, sexual function, and fertility. Managing atypical genitalia often requires a team of specialists, including:
-
Pediatricians and neonatologists
-
Pediatric urologists and surgeons
-
Endocrinologists and medical geneticists
-
Psychologists or social workers
Medicines
Hormone therapy may be used to correct or manage hormonal imbalances.
-
Example: In genetic females with mild congenital adrenal hyperplasia, hormone replacement may normalize genital development.
Surgery
Surgery may be performed to:
-
Maintain healthy sexual function
-
Create genitals that appear more typical
Timing of surgery depends on the child’s situation. Some professionals recommend delaying cosmetic-only surgery until the child can participate in decisions.
Surgical goals include:
-
For girls: Exposing hidden vaginal openings to ensure sexual function later
-
For boys: Reconstructing partially developed penis and placing testicles in the scrotum
Risks and outcomes:
-
Surgery is often satisfying, but repeat procedures may be required
-
Risks include disappointing appearance or impaired sexual function
Ongoing Care
Children with atypical genitalia require lifelong follow-up:
-
Regular checkups to monitor growth and development
-
Cancer screenings if indicated
-
Hormonal and reproductive health monitoring
Advertisement