Overview
Diagnosis
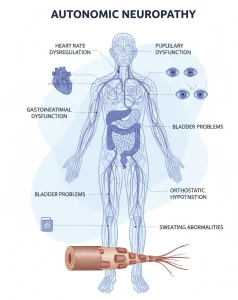
Autonomic neuropathy may develop as a complication of several diseases. The tests required depend on your symptoms and risk factors.
For people with risk factors:
-
If you have diabetes or another condition that increases your risk, your healthcare provider will do a physical exam and review your symptoms.
-
If you are undergoing cancer treatment with a drug known to cause nerve damage, your provider will monitor for signs of neuropathy.
For people without risk factors:
-
Diagnosis may require a more detailed assessment. Your provider will review your medical history, discuss symptoms, and perform a physical exam.
-
Tests may include:
-
Autonomic function tests: Measure heart rate and blood pressure response during exercises like deep breathing or the Valsalva maneuver.
-
Tilt-table test: Monitors blood pressure and heart rate as your position changes. A simple version measures blood pressure lying, sitting, and standing; another involves standing, squatting, and standing again while monitoring cardiovascular responses.
-
Gastrointestinal tests: Gastric-emptying tests evaluate digestive issues such as gastroparesis.
-
Quantitative sudomotor axon reflex test: Measures how nerves controlling sweat glands respond to stimulation using small electrical currents.
-
Thermoregulatory sweat test: Powder changes color when you sweat. Photos track sweat patterns in a heated chamber to confirm diagnosis.
-
Urinalysis and urodynamic tests: Evaluate bladder function if urinary symptoms are present.
-
Ultrasound: High-frequency sound waves create images of the bladder and urinary tract.
-
Treatment
Treatment aims to manage the underlying disease and relieve symptoms based on which parts of the body are affected.
Managing underlying disease:
-
Control the disease causing nerve damage, such as tight blood sugar control in diabetes.
-
About 50% of cases may have no identifiable cause.
Digestive (gastrointestinal) symptoms:
-
Diet changes: Increase fiber and fluid intake. Fiber supplements like Metamucil or Citrucel may help.
-
Medications to aid stomach emptying: Metoclopramide (Reglan) increases digestive contractions. Short-term use is recommended.
-
Constipation relief: Over-the-counter laxatives as advised by your provider.
-
Diarrhea management: Antibiotics or anti-diarrheal medications may help.
Urinary symptoms:
-
Bladder retraining: Scheduled fluid intake and urination to improve bladder control.
-
Medications: Drugs to manage overactive bladder or aid complete emptying.
-
Catheterization: Tube inserted through the urethra to empty the bladder.
Sexual dysfunction:
-
For men:
-
Medications: Sildenafil (Viagra), Vardenafil, Tadalafil (Cialis), Avanafil (Stendra). Caution in heart disease, arrhythmia, stroke, high blood pressure, or nitrate use. Seek immediate care for erections lasting over 4 hours.
-
External vacuum pump: Hand pump pulls blood into the penis, maintained by a tension ring.
-
-
For women:
-
Vaginal lubricants: Reduce dryness for more comfortable intercourse.
-
Medications for low sexual desire: Approved options exist for premenopausal women.
-
Heart rhythm and blood pressure symptoms:
-
High-salt, high-fluid diet: Helps maintain blood pressure when standing; use cautiously in heart failure.
-
Compression garments: Waist binders or thigh-high stockings improve blood flow.
-
Medications to raise blood pressure:
-
Fludrocortisone: Retains salt to regulate blood pressure.
-
Midodrine (Orvaten), Droxidopa (Northera): Raise standing blood pressure but may cause high pressure when lying down.
-
Octreotide (Sandostatin): For postprandial low blood pressure in diabetes.
-
Pyridostigmine (Mestinon): Helps maintain stable standing blood pressure.
-
-
Medications to regulate heart rate: Beta blockers control high heart rate during activity.
Sweating abnormalities:
-
Excess sweating: Medications like Glycopyrrolate (Cuvposa, Robinul) reduce sweat. Side effects may include diarrhea, dry mouth, blurred vision, heart rate changes, headache, loss of taste, drowsiness. Reduced sweating can increase heat-related illness risk.
Advertisement