Overview
Diagnosis
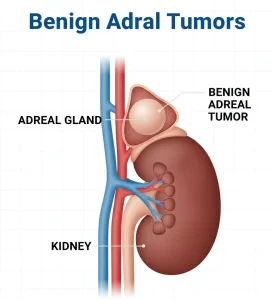
Benign adrenal tumors are typically found by chance on imaging tests. Once detected, a healthcare professional evaluates:
-
Cancer risk: Determining whether the tumor has characteristics that suggest malignancy.
-
Hormone production: Checking if the tumor secretes excess hormones, which can affect blood pressure, metabolism, and other bodily functions.
Diagnostic tests may include:
-
Blood and urine tests: Assess for excess hormones and identify the specific hormone being produced.
-
Imaging studies: Provide detailed information about the tumor’s size, location, and cancer risk.
Imaging options include:
-
CT scan: Produces cross-sectional X-ray images for detailed visualization of the adrenal gland.
-
MRI: Uses radio waves and magnetic fields to generate high-resolution images.
-
M-iodobenzylguanidine (MIBG) scan: A radioactive compound highlights tumors that take up the substance, identifying even small growths.
-
Positron emission tomography (PET): Detects tumors that absorb radioactive compounds.
-
Ga-DOTATATE PET scanning: Advanced imaging, often combined with CT or MRI, for identifying endocrine system tumors; availability may be limited.
Treatment
Many benign adrenal tumors do not require immediate treatment. Decisions are based on:
-
Hormone production
-
Tumor growth or symptoms
-
Risk of malignancy
Management strategies include:
-
Active surveillance (watchful waiting):
-
Small, non-hormone-producing tumors may be monitored with repeat imaging at 3–6 months after diagnosis, then every 1–2 years.
-
Hormone levels may be checked annually for up to 5 years.
-
-
Medication management:
-
For tumors causing hormone-related symptoms, medications may help control conditions like high blood pressure before surgery.
-
-
Surgery (adrenalectomy):
-
Removal of the adrenal gland may be necessary if the tumor grows, causes symptoms, or has a higher risk of cancer.
-
Laparoscopic surgery is often used for small, low-risk tumors.
-
Advertisement