Overview
Diagnosis of Bladder Exstrophy
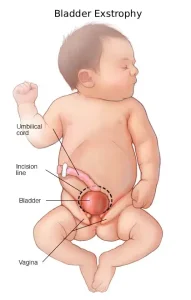
Bladder exstrophy (BE) is often discovered by chance during a routine pregnancy ultrasound, though it can sometimes be identified after birth. Diagnosis may involve:
-
Prenatal Imaging: High-resolution ultrasound or fetal MRI can reveal signs such as:
-
A bladder that doesn’t fill or empty correctly
-
Low placement of the umbilical cord
-
Separated pubic bones
-
Smaller-than-typical genitals
-
-
Newborn Examination: If not detected before birth, healthcare professionals check for:
-
The size of the exposed bladder portion
-
Testicle positioning
-
Intestine bulging through the abdominal wall (inguinal hernia)
-
Navel anatomy
-
Pubic bone separation and pelvic mobility
-
Position of the anus
-
Mayo Clinic’s fetal care center offers advanced imaging and prenatal management for babies with urology conditions, allowing parents to meet the care team before birth.
Treatment of Bladder Exstrophy
Treatment for bladder exstrophy is surgical, often called reconstructive surgery, and aims to:
-
Provide adequate urine storage space
-
Create functional and cosmetically acceptable outer sex organs
-
Establish bladder control (continence)
-
Support kidney function
If the condition is detected before birth, surgical planning often occurs immediately after delivery. If found postnatally, the newborn may be treated in a specialized hospital unit or transferred to a center experienced in bladder exstrophy. A clear plastic dressing is used to protect the exposed bladder until surgery.
Types of Bladder Exstrophy Surgery
There are two main surgical approaches, with ongoing research to refine outcomes:
-
Complete Primary Repair:
-
The bladder, abdominal wall, urethra, and outer sex organs are repaired in a single surgery.
-
Surgery can be done soon after birth or at 2–3 months of age.
-
Pelvic bone repair may be included if the infant is older than 72 hours, or if separation is significant.
-
-
Modern Staged Repair:
-
Three separate surgeries are performed:
-
Within 72 hours after birth – closure of the bladder and abdominal wall
-
At 6–12 months – urethra and sex organ repair
-
At 4–5 years – bladder neck and muscle repair for continence
-
-
Surgical Follow-Up
Post-surgery care focuses on healing and long-term bladder function:
-
Immobilization: Devices keep the lower legs still during healing (usually 4–6 weeks).
-
Pain Management: A spinal catheter may deliver consistent pain relief, reducing the need for opioids.
-
Bladder Control: Some children achieve partial control; additional bladder neck surgery may improve continence.
-
Catheterization: Some children may require a tube to drain urine temporarily.
-
Further Surgeries: Additional procedures may be needed over time to improve urination or repair genitals as the child grows.
Advertisement