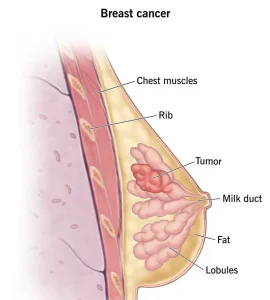
Overview
Diagnosis of Breast Cancer
Breast cancer diagnosis usually begins with an exam and discussion of symptoms. Imaging tests and tissue samples help confirm whether cancer is present.
-
Breast exam: A healthcare professional checks the breasts for skin changes, nipple changes, or lumps. Lymph nodes along the collarbones and armpits are also examined.
-
Mammogram: An X-ray of the breast tissue.
-
Screening mammogram: Routine check to detect early cancer.
-
Diagnostic mammogram: Detailed imaging to closely examine areas of concern.
-
-
Breast ultrasound: Uses sound waves to create images. Helps distinguish between solid masses and fluid-filled cysts.
-
Breast MRI: Uses magnetic fields and radio waves to create detailed images.
-
Dye may be injected to highlight tissue.
-
Can detect additional cancer areas in the affected or opposite breast.
-
-
Core needle biopsy: A needle removes a tissue sample for lab testing, often with a marker placed to track the site.
Laboratory Testing
-
Determines cancer presence
-
Identifies cancer type and growth rate
-
Tests for hormone receptors to guide treatment planning
Staging Breast Cancer
Staging shows the extent of cancer and helps plan treatment.
-
Tests may include:
-
Blood tests (complete blood count, kidney/liver function)
-
Bone scan
-
CT scan
-
MRI
-
PET scan
-
Breast cancer stages (0–4):
-
Stage 0: Cancer contained within a duct.
-
Stage 1–3: Increasing invasion into breast tissue and lymph nodes.
-
Stage 4: Cancer has spread to other parts of the body.
Treatment of Breast Cancer
Treatment depends on cancer type, stage, growth rate, hormone sensitivity, and overall health.
Surgery
-
Lumpectomy: Removes cancer and surrounding tissue, preserves most of the breast. Often combined with radiation therapy.
-
Mastectomy: Removes all breast tissue; includes:
-
Total/simple mastectomy
-
Skin-sparing mastectomy
-
Nipple-sparing mastectomy
-
-
Lymph node removal:
-
Sentinel node biopsy: Removes a few nodes to check for cancer spread.
-
Axillary lymph node dissection: Removes many nodes if cancer has spread.
-
-
Contralateral prophylactic mastectomy: Optional removal of the other breast in high-risk patients.
-
Breast reconstruction: Surgery to restore breast shape using implants or tissue.
Risks of surgery: Pain, bleeding, infection, lymphedema (arm swelling).
Radiation Therapy
-
Uses X-rays, protons, or brachytherapy to kill remaining cancer cells.
-
Often follows surgery to lower recurrence risk.
Side effects: Fatigue, rash, breast swelling, rare heart/lung damage, possible secondary cancers.
Chemotherapy
-
Uses strong medicines to kill cancer cells.
-
Can be given before or after surgery.
-
Helps shrink tumors, treat lymph node involvement, and control metastatic cancer.
Side effects: Hair loss, nausea, vomiting, fatigue, infection risk, premature menopause, nerve damage.
Hormone Therapy
-
For cancers sensitive to estrogen and progesterone.
-
Blocks hormones from fueling cancer growth.
Types of hormone therapy:
-
Selective estrogen receptor modulators (SERMs)
-
Aromatase inhibitors
-
Surgery or medicines to stop ovarian hormone production
Side effects: Hot flashes, night sweats, vaginal dryness, bone thinning, blood clots.
Targeted Therapy
-
Attacks specific cancer cell proteins, e.g., HER2-positive breast cancer.
-
Can be used before surgery, after surgery, or for metastatic cancer.
Immunotherapy
-
Helps the immune system detect and destroy cancer cells.
-
Often used for triple-negative breast cancer.
Palliative Care
-
Focuses on relieving pain and symptoms of serious illness.
-
Provides an extra layer of support alongside treatments like surgery, chemotherapy, and radiation.
-
Can improve quality of life and longevity when combined with standard treatments.
Advertisement