Overview
Diagnosis
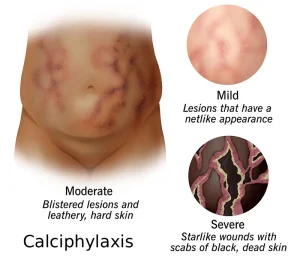
Diagnosing Calciphylaxis requires a careful evaluation of skin changes, medical history, and laboratory findings. Because this condition can resemble other skin disorders, early and accurate diagnosis is critical for effective treatment.
Common diagnostic methods include:
-
Physical examination:
A doctor will examine the affected skin areas for painful, purplish lesions or ulcers, typically found on the thighs, abdomen, or buttocks. These skin lesions are often the first visible sign of calciphylaxis. -
Skin biopsy:
This is the most definitive diagnostic test. A small piece of affected skin is removed and examined under a microscope to detect calcium deposits in small blood vessels, tissue necrosis, and other characteristic changes. -
Blood tests:
Laboratory tests are used to check calcium, phosphate, parathyroid hormone (PTH), and kidney function levels, as imbalances in these can contribute to calciphylaxis. -
Imaging tests:
In some cases, X-rays or bone scans may be performed to identify calcium buildup in soft tissues or blood vessels.
Treatment
Treatment for Calciphylaxis focuses on managing pain, preventing infection, improving blood flow, and correcting mineral imbalances. Because this condition is often linked to kidney failure and abnormal calcium-phosphate metabolism, a multidisciplinary approach is essential.
Main treatment options include:
-
Correction of mineral imbalance:
Doctors work to reduce high calcium and phosphate levels in the blood. This may involve dietary restrictions, phosphate binders, and adjusting doses of vitamin D or calcium supplements. -
Sodium thiosulfate therapy:
This intravenous medication helps dissolve calcium deposits and improve blood vessel function. It’s commonly used as a first-line treatment in calciphylaxis. -
Pain management:
Calciphylaxis causes intense pain. Opioid pain relievers or other medications may be prescribed for symptom control. -
Wound care:
Proper wound care is critical to prevent infection and promote healing. This includes regular dressing changes, debridement, and use of topical or systemic antibiotics when infection occurs. -
Dialysis modification:
For patients on dialysis, treatment plans may be adjusted to improve calcium and phosphate control. -
Surgery:
In severe cases, surgical removal of necrotic tissue or parathyroidectomy (removal of the parathyroid glands) may be required if other treatments fail.
Prevention and Management
Since calciphylaxis is rare but life-threatening, prevention focuses on controlling risk factors and maintaining mineral balance, especially in patients with chronic kidney disease.
Preventive measures include:
-
Monitoring calcium and phosphate levels regularly.
-
Avoiding excessive vitamin D or calcium supplementation.
-
Maintaining optimal dialysis efficiency.
-
Treating underlying conditions like diabetes and obesity.
-
Quitting smoking and improving nutrition to support vascular health.
Key Takeaway
Calciphylaxis is a serious vascular disorder characterized by calcium buildup in small blood vessels, leading to painful skin lesions and a high risk of infection. Early diagnosis, aggressive wound care, and management of calcium-phosphate imbalance can significantly improve outcomes and survival rates.
Advertisement