Overview
Diagnosis of Cavities (Tooth Decay)
To diagnose tooth decay or dental cavities, your dentist will evaluate your symptoms, examine your mouth, and may perform imaging tests to determine the extent of damage.
During a dental checkup, your dentist may:
-
Ask about pain or sensitivity in your teeth.
-
Inspect your teeth and gums for visible signs of decay.
-
Use dental instruments to gently probe for soft or weakened areas.
-
Take dental X-rays to reveal cavities hidden between teeth or under the surface.
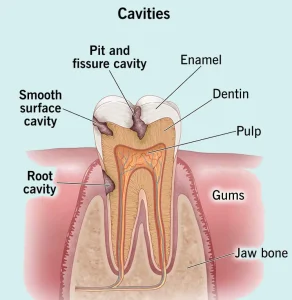
Based on findings, your dentist will identify the type of cavity you have — smooth surface, pit and fissure, or root cavity.
Types of Cavities
Smooth Surface Cavities
Form on the flat surfaces of teeth. Usually progress slowly and can sometimes be reversed with fluoride treatment.
Pit and Fissure Cavities
Develop in the grooves and crevices of molars and premolars. Common in children and teens who may not clean back teeth thoroughly.
Root Cavities
Occur when gums recede, exposing the tooth root. The root surface is softer and more prone to decay.
Treatment for Cavities
Early diagnosis is key to preventing serious dental problems. Treating tooth decay early can save your natural teeth and reduce the need for complex procedures.
Fluoride Treatments
Recommended for very early-stage cavities. Professional fluoride applications (gel, varnish, or foam) help remineralize enamel and stop decay progression.
Fillings (Dental Restorations)
The most common treatment for cavities. Dentists remove decayed material and fill the area using composite resin, porcelain, or amalgam materials.
Dental Crowns
Used when there is extensive decay or weakened tooth structure. The damaged area is removed, and a custom crown (made of porcelain, gold, or metal) covers the remaining tooth for protection.
Root Canal Treatment
Required when decay reaches the pulp (tooth’s inner nerve). The infected pulp is removed, the canal is cleaned, disinfected, and filled to preserve the tooth.
Tooth Extraction
In cases of severe decay where the tooth can’t be saved. The removed tooth may be replaced with a dental implant, bridge, or partial denture to prevent shifting of nearby teeth.
Preparing for Your Dental Appointment
If you’re experiencing tooth pain or sensitivity, schedule a dental visit promptly. Before your appointment, prepare by:
-
Listing all medications, supplements, and allergies.
-
Bringing any mouthguards or dental devices you use.
-
Preparing questions for your dentist, such as:
-
Do I need a filling, crown, or root canal?
-
How long will recovery take?
-
How can I prevent future cavities?
-
Does my local water supply contain fluoride?
-
What to Expect from Your Dentist
Your dentist may ask questions like:
-
Do sweet, hot, or cold foods cause pain?
-
Does biting increase your discomfort?
-
How often do you brush and floss?
-
Do you use fluoride toothpaste?
-
Do you frequently eat sugary foods or drink soda?
-
Have you experienced dry mouth?
-
What medications are you taking?
Answering these questions accurately helps your dentist tailor the best treatment for you.
Managing Tooth Pain Before Your Appointment
While waiting to see your dentist, you can ease discomfort by:
-
Taking over-the-counter pain relievers (as advised by your healthcare provider).
-
Using numbing gels for temporary relief.
-
Brushing with warm water and sensitive-teeth toothpaste.
-
Keeping your mouth clean — avoid skipping painful areas.
-
Avoiding hot, cold, or sugary foods that trigger pain.
Key Takeaway
Cavities are preventable and treatable with early detection. Regular dental visits, good oral hygiene, and fluoride use are essential to maintaining healthy teeth. If you notice pain, sensitivity, or discoloration, see your dentist immediately to prevent further damage.
Advertisement