Overview
Diagnosis
Many people with celiac disease are unaware they have it because symptoms can be subtle or mistaken for other digestive problems. To diagnose celiac disease accurately, several tests may be performed — ideally before starting a gluten-free diet, as eliminating gluten can interfere with test results.
1. Blood Tests
-
Serology Testing: Detects specific antibodies that react to gluten. Elevated levels indicate an immune response consistent with celiac disease.
-
Genetic Testing: Looks for the presence of HLA-DQ2 and HLA-DQ8 genes. While not diagnostic on their own, their absence can effectively rule out celiac disease.
2. Endoscopy
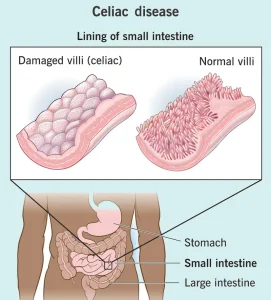
A small camera on a flexible tube is inserted through the mouth to examine the upper digestive tract. During the procedure, a biopsy (tiny tissue sample) is taken from the small intestine to check for damage to the villi — the finger-like structures responsible for nutrient absorption.
3. Capsule Endoscopy
Used when a full view of the small intestine is needed. You swallow a vitamin-sized capsule containing a miniature wireless camera that captures thousands of images as it passes through your digestive system.
4. Skin Biopsy
If you have a related rash known as dermatitis herpetiformis, your healthcare professional may remove a small sample of skin to check for signs of celiac disease under a microscope.
5. Additional Nutritional Testing
Once diagnosed, your healthcare team may test for nutritional deficiencies, including levels of:
-
Vitamins A, B-12, D, and E
-
Iron, zinc, copper, and folic acid
-
Hemoglobin and liver enzymes
Bone density scans may also be performed to evaluate bone health.
Treatment
The only effective treatment for celiac disease is a lifelong, strict gluten-free diet. Even tiny amounts of gluten can cause intestinal damage.
Foods Containing Gluten
Avoid products made from:
-
Wheat (including spelt and durum)
-
Barley
-
Rye
-
Malt
-
Bulgur
-
Semolina
-
Triticale
-
Graham flour
-
Farina
A registered dietitian experienced with celiac disease can help create a balanced, gluten-free meal plan.
Hidden Sources of Gluten
Gluten may be found in:
-
Processed foods with modified starches or stabilizers
-
Medicines, vitamins, and herbal supplements
-
Lipsticks, toothpaste, and mouthwash
-
Communion wafers and glue on stamps or envelopes
-
Play dough and some cosmetic products
Vitamin and Mineral Supplements
If nutrient deficiencies are present, supplements may be prescribed for:
-
Iron
-
Vitamin B-12
-
Vitamin D
-
Vitamin K
-
Copper
-
Folic acid
-
Zinc
If absorption is poor, injections may be needed instead of pills.
Follow-Up Care
Regular follow-ups are crucial to ensure recovery and prevent complications:
-
Blood tests are done periodically to monitor antibody levels.
-
Nutrient levels are checked to confirm improvement.
-
Endoscopy with biopsy may be repeated if symptoms persist or return.
Children typically recover within 3–6 months, while adults may take several years for complete intestinal healing.
Medicines for Inflammation
If the intestine remains severely inflamed or if refractory celiac disease develops, medications may include:
-
Corticosteroids (to control inflammation temporarily).
-
Azathioprine (Imuran) or Budesonide (Entocort EC, Uceris) in resistant cases.
Treating Dermatitis Herpetiformis
For celiac-related skin rashes, Dapsone may be prescribed alongside a gluten-free diet. Regular blood monitoring is required to check for side effects.
Refractory Celiac Disease
This rare form occurs when the small intestine doesn’t heal despite a gluten-free diet. It can be serious and requires care from a specialized medical center experienced in treating advanced celiac disease.
Advertisement