Overview
Diagnosis
Asthma in children can be challenging to diagnose because its symptoms can resemble other conditions. A healthcare professional considers your child’s symptoms, medical history, and may recommend tests to confirm the diagnosis and rule out other causes.
Common diagnostic tests include:
-
Lung function tests: Spirometry measures how much air a child can exhale and how quickly. These tests may be done at rest, after exercise, or after using asthma medicine. A peak flow meter can also measure how strongly your child exhales.
-
Bronchoprovocation test: Uses spirometry to assess how the lungs respond to triggers such as exercise or cold air.
-
Exhaled nitric oxide test: Measures nitric oxide levels in the breath to help determine airway inflammation and whether steroid medicines may be beneficial.
-
Allergy tests: Skin tests may identify allergic triggers such as pollen, dust mites, mold, or pet dander.
For children under 5, these tests may not be accurate. In such cases, healthcare professionals often rely on symptoms and a trial of asthma medicine to observe the response. Sometimes, a clear diagnosis can only be made after months or years of monitoring.
Conditions that look like asthma
Other conditions that can cause similar symptoms include:
-
Rhinitis
-
Sinusitis
-
Acid reflux (GERD)
-
Airway or breathing problems
-
Bronchiolitis or respiratory infections such as RSV
A healthcare professional will evaluate whether asthma, another condition, or a combination of both is responsible for the symptoms.
Treatment
Asthma treatment focuses on keeping symptoms under control and preventing flare-ups. The goal is to ensure that your child has:
-
Minimal or no symptoms
-
Few or no flare-ups
-
No limits on physical activity
-
Minimal need for rescue inhalers
-
Few or no medicine side effects
If an infant or toddler has frequent or severe wheezing, a trial of asthma medicine may be used to see if symptoms improve.
Long-term control medicines
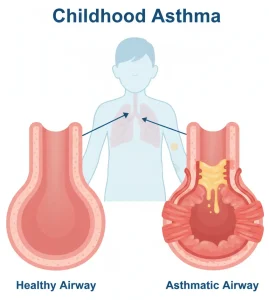
These medicines reduce airway inflammation and are taken daily to prevent symptoms.
-
Inhaled corticosteroids: Examples include fluticasone, budesonide, mometasone, ciclesonide, and beclomethasone. It may take several days or weeks to see full benefits. Long-term use may slightly slow growth, but the benefits outweigh the risks.
-
Leukotriene modifiers: Oral medicines such as montelukast and zafirlukast prevent asthma symptoms for up to 24 hours.
-
Combination inhalers: Contain both a corticosteroid and a long-acting beta agonist (LABA), such as fluticasone and salmeterol, or budesonide and formoterol. These are prescribed only when asthma is not well controlled by other medicines.
-
Biologics: Injectable medicines such as mepolizumab, dupilumab, benralizumab, omalizumab, and tezepelumab may be used for children with severe asthma.
Quick-relief medicines
These medicines open swollen airways quickly and are used during asthma attacks or before exercise.
-
Short-acting beta agonists (SABAs): Inhaled medicines like albuterol and levalbuterol act within minutes and provide relief for several hours.
-
Oral or intravenous corticosteroids: Used short-term to treat severe asthma attacks but not recommended for long-term use due to potential side effects.
Treatment for allergy-induced asthma
When allergies trigger asthma symptoms, additional treatments may help:
-
Omalizumab: An injectable medicine given every four weeks for severe allergic asthma.
-
Allergy medicines: Include oral or nasal antihistamines and decongestants.
-
Immunotherapy: Allergy shots or tablets that gradually reduce sensitivity to allergens.
Don’t rely only on quick-relief medicines
Quick-relief inhalers provide immediate help, but long-term control medicines are essential for managing asthma effectively. If your child uses a rescue inhaler frequently, see a healthcare professional to adjust the long-term treatment plan.
Inhaled medicine devices
Different devices help children take asthma medicines correctly:
-
Older children may use metered dose or dry powder inhalers.
-
Infants and toddlers use a face mask with a metered dose inhaler or nebulizer.
-
Babies typically use a nebulizer that turns liquid medicine into mist for easy inhalation.
Asthma action plan
Work with your child’s healthcare provider to create a written asthma action plan. It helps you:
-
Adjust medicines as needed
-
Track symptoms and peak flow readings
-
Recognize early warning signs of an asthma attack
-
Know when to seek medical help
Peak flow meters can be used by older children to measure breathing strength. The action plan may divide asthma control into zones — green for good control, yellow for caution, and red for medical alert.
Because asthma symptoms and triggers can change over time, regular checkups are important. If your child’s symptoms are well controlled, the provider may recommend lowering medicine doses (step-down treatment). If symptoms worsen, medicine adjustments may be needed (step-up treatment).
Advertisement