Overview
Diagnosis
Tests and procedures used to diagnose chronic myelogenous leukemia help confirm the disease, identify the presence of genetic changes, and determine how advanced it is.
A physical exam includes checking your pulse, blood pressure, and the size of your lymph nodes, spleen, and abdomen. Your healthcare provider may look for swelling or tenderness in these areas.
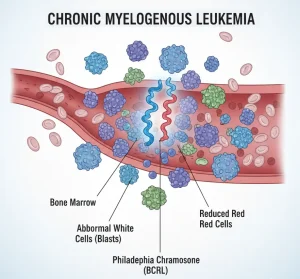
Blood tests are used to measure the number and types of cells in your blood. A complete blood count, or CBC, can show a very high number of white blood cells, which is common in chronic myelogenous leukemia. Blood samples may also be tested to check how well your organs are functioning.
Bone marrow tests help confirm the diagnosis and measure the extent of the disease. A bone marrow aspiration collects the liquid part of the marrow, while a biopsy collects a small piece of solid tissue. Both samples are usually taken from the hip bone and sent to a lab for analysis.
Specialized genetic tests are used to look for the Philadelphia chromosome or the BCR-ABL gene, which are markers of chronic myelogenous leukemia. These may include fluorescence in situ hybridization (FISH) and polymerase chain reaction (PCR) tests.
Phases of chronic myelogenous leukemia
Chronic myelogenous leukemia develops in different phases based on how aggressive the disease is. The phase depends on the ratio of diseased cells to healthy cells in the blood or bone marrow.
• Chronic phase – The earliest and most treatable phase, where symptoms are often mild and response to therapy is best.
• Accelerated phase – The disease becomes more aggressive, and the number of abnormal cells increases.
• Blast phase – The most advanced phase, where the disease behaves like an acute leukemia and becomes life-threatening.
Treatment
The main goal of treatment for chronic myelogenous leukemia is to eliminate blood cells that contain the BCR-ABL gene. Most people begin with targeted therapy to help achieve long-term remission.
Targeted therapy
Targeted therapy focuses on blocking the specific proteins that cause cancer cells to grow. In chronic myelogenous leukemia, medicines known as tyrosine kinase inhibitors (TKIs) target the abnormal protein produced by the BCR-ABL gene.
TKIs are the first-line treatment for most people. Common side effects include swelling or puffiness of the skin, nausea, diarrhea, fatigue, muscle cramps, and skin rashes.
Regular blood tests are used to monitor how well targeted therapy is working by measuring the BCR-ABL gene levels. If the disease does not respond or becomes resistant, other targeted medicines or alternative treatments may be considered.
Because it is not yet clear when it is completely safe to stop targeted therapy, most people continue taking TKIs even after reaching remission. In some cases, your healthcare provider may discuss stopping therapy after weighing the potential risks and benefits.
Bone marrow transplant
A bone marrow transplant, also called a stem cell transplant, is the only known cure for chronic myelogenous leukemia. It is usually reserved for people whose disease does not respond to other treatments.
The procedure involves using high doses of chemotherapy to destroy the diseased bone marrow. Donor stem cells are then infused into the bloodstream to rebuild healthy blood cells.
Although a bone marrow transplant can be curative, it carries a high risk of serious complications and side effects.
Chemotherapy
Chemotherapy uses strong medicines to kill leukemia cells and may be combined with targeted therapy in aggressive forms of chronic myelogenous leukemia.
Side effects vary depending on the medicines used and may include nausea, fatigue, and low blood cell counts.
Advertisement