Overview
Diagnosis
People with early-stage cirrhosis often have no symptoms. The condition is sometimes first detected during a routine blood test or an exam done for another reason. To confirm a diagnosis, healthcare professionals use a combination of laboratory and imaging tests.
Lab tests
Blood tests check for signs of liver malfunction, such as increased bilirubin levels and elevated liver enzymes. Tests also measure kidney function by checking creatinine levels, screen for hepatitis viruses, and assess blood clotting with a prothrombin or INR test. Together, these results help confirm cirrhosis and may also show its stage and cause.
Imaging tests
Noninvasive imaging such as transient elastography or magnetic resonance elastography (MRE) can show liver stiffness or hardening. Other imaging options include MRI, CT scans, or ultrasound to evaluate liver structure and detect complications.
Biopsy
A liver biopsy may be performed to determine the extent of liver damage and identify its cause. However, it’s not always required for diagnosis.
After a cirrhosis diagnosis, ongoing monitoring is essential. Regular tests help track disease progression and detect complications such as esophageal varices and liver cancer. Noninvasive monitoring methods are increasingly used to reduce the need for frequent biopsies.
Treatment
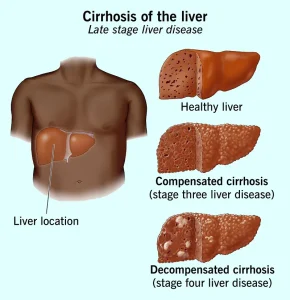
Cirrhosis treatment depends on the underlying cause and the level of liver damage. The main goals are to slow the progression of scarring, manage symptoms, and prevent complications. Reversing cirrhosis is generally not possible. In severe cases, hospitalization may be needed.
Treating the underlying cause
In the early stages, liver damage can sometimes be slowed or controlled by addressing the root cause.
• Alcohol dependency treatment – Stopping alcohol use is essential for people whose cirrhosis is caused by heavy drinking. A treatment program may be recommended for support.
• Weight loss and metabolic control – For cirrhosis linked to metabolic dysfunction-associated steatotic liver disease, weight loss and managing blood sugar levels can improve liver health.
• Hepatitis treatment – Antiviral medicines can help control hepatitis B or C and prevent further liver damage.
• Medicines for specific liver diseases – Certain types of cirrhosis, such as primary biliary cholangitis, may respond to medicines that slow disease progression.
• Symptom management and nutrition – Medicines can help relieve symptoms such as itching or fatigue. Nutritional supplements and vitamins may treat malnutrition or prevent bone loss (osteoporosis).
Treating complications
Managing complications is a key part of cirrhosis care.
• Fluid buildup (ascites and swelling) – A low-sodium diet and diuretics may help reduce fluid retention. Severe cases might need drainage procedures or surgery.
• Portal hypertension – Blood pressure medicines may reduce pressure in the liver veins and prevent bleeding. Endoscopy can detect varices (enlarged veins), and treatments such as band ligation or a transjugular intrahepatic portosystemic shunt (TIPS) can reduce bleeding risk.
• Infections – Antibiotics may be prescribed, and vaccinations for influenza, pneumonia, and hepatitis are recommended.
• Liver cancer monitoring – Regular blood tests and ultrasounds are used to detect early signs of liver cancer.
• Hepatic encephalopathy – Medicines can help remove toxins from the blood to reduce confusion or other mental symptoms.
Liver transplant
When cirrhosis progresses to advanced liver failure, a liver transplant may be the only effective treatment. The damaged liver is replaced with a healthy liver from a deceased or living donor. Cirrhosis is one of the most common reasons for liver transplantation.
Candidates must undergo extensive evaluation to ensure good post-surgery outcomes. Carefully selected people with alcoholic cirrhosis can have transplant results similar to those with other liver diseases.
To be considered for a transplant due to alcoholic cirrhosis, individuals must:
• Find a program that accepts and supports patients with alcoholic cirrhosis.
• Commit to lifelong alcohol abstinence and meet all program-specific requirements.
Potential future treatments
Researchers are developing new approaches to slow or reverse liver scarring. Future treatments may include:
• Targeted therapies that act directly on liver cells
• Improved early screening and lifestyle interventions
• Medicines designed to prevent fibrosis progression
Although these treatments are not yet available, early detection and consistent care remain key to managing cirrhosis effectively.
Advertisement