Overview
Diagnosis
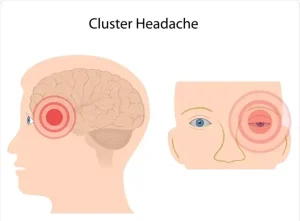
Cluster headache has a distinctive type of pain and attack pattern. Diagnosis depends on describing the location, intensity, and nature of the pain, as well as other symptoms. The frequency and duration of the headaches also play an important role.
A neurologist, who specializes in brain and nervous system conditions, typically diagnoses cluster headache based on medical history, symptoms, and a physical and neurological examination.
For people with unusual or complicated headaches, diagnostic tests may be done to rule out other causes. These include:
-
MRI scan – Uses a powerful magnetic field and radio waves to create detailed images of the brain and blood vessels. It helps detect tumors, strokes, bleeding, infections, and other neurological conditions.
-
CT scan – Uses X-rays to produce detailed cross-sectional images of the brain. It helps diagnose tumors, infections, brain injuries, bleeding, and other possible medical issues that may cause headaches.
More Information
-
Cluster headache care at Mayo Clinic
-
Brain CT scan
-
Brain magnetic resonance imaging
Treatment
There is currently no cure for cluster headaches. The goal of treatment is to reduce pain, shorten the cluster period, and prevent future attacks. Because the pain comes on suddenly and ends quickly, fast-acting treatments are essential.
Fast-Acting Treatments
These therapies aim to stop a cluster headache once it begins:
-
Oxygen – Breathing pure oxygen through a mask provides relief within about 15 minutes for most people. It is safe but not suitable for those with severe chronic obstructive pulmonary disease.
-
Triptans – Sumatriptan injections work quickly to relieve pain. Nasal sprays such as sumatriptan or zolmitriptan are also effective but act more slowly. Triptans are not recommended for people with heart disease or uncontrolled high blood pressure.
-
Octreotide (Sandostatin) – A synthetic form of the hormone somatostatin that may relieve pain in people who do not respond to triptans.
-
Local anesthetics – Nasal application of lidocaine may reduce pain for some people.
-
Dihydroergotamine – Given intravenously, this medicine can relieve cluster headache pain. An inhaled nasal form exists but has not been proven effective for cluster headaches.
Preventive Treatments
Preventive therapy begins at the start of a cluster period to stop or lessen attacks. Once the cluster phase ends, medication is tapered off.
Common preventive treatments include:
-
Calcium channel blockers – Verapamil is the first-choice medicine and may be combined with others for better results. Possible side effects include constipation, fatigue, nausea, and irregular heartbeat.
-
Corticosteroids – Prednisone and similar drugs work quickly to relieve pain and are used for short periods or during brief cluster bouts. Long-term use may cause diabetes, high blood pressure, or osteoporosis.
-
Galcanezumab (Emgality) – A newer medicine approved for episodic cluster headache, given as a monthly injection until the cluster period ends.
-
Lithium (Lithobid) – Used mainly for chronic cluster headache or when other medicines fail. Regular blood tests are needed to monitor kidney function and side effects such as tremor and increased thirst.
-
Noninvasive vagus nerve stimulation (VNS) – A handheld device that sends mild electrical impulses to the vagus nerve through the skin, which may reduce attack frequency.
-
Nerve block – An injection of anesthetic and corticosteroid around the occipital nerve at the back of the head, providing short-term relief until preventive medications take effect.
Other preventive medicines may include anti-seizure drugs such as topiramate.
Surgery
Surgery is rarely needed and is reserved for people who do not respond to other treatments. Some procedures target nerve pathways involved in the pain mechanism. However, results are uncertain and may cause complications such as facial numbness or jaw weakness.
Neuromodulation
Neuromodulation involves using electrical stimulation to alter nerve activity and reduce pain. Techniques include sphenopalatine ganglion stimulation, occipital nerve stimulation, and deep brain stimulation.
These procedures involve implanting a device that sends controlled electrical impulses to specific brain areas to block pain signals. Early studies show promise, especially with occipital nerve stimulation, for people who do not respond to medications. More research is ongoing to confirm long-term effectiveness.
Advertisement