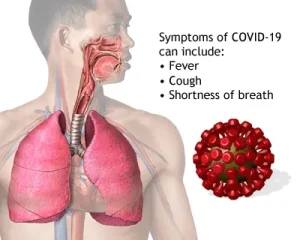
Overview
Diagnosis
If you have symptoms of COVID-19 or have been exposed to someone infected with the virus, contact your healthcare provider. Inform them about any close contact with confirmed cases.
In the United States, at-home COVID-19 tests approved or authorized by the U.S. Food and Drug Administration (FDA) are available. You can visit the FDA website to check the list of validated tests and their expiration dates. Always read and follow the test’s instructions carefully for the most accurate results.
When to Test for COVID-19
-
If you have symptoms: Test immediately.
-
If you were exposed but have no symptoms: Wait at least 5 days after exposure before testing.
-
If you tested positive within the last 30 days:
-
If you have symptoms, you can test again.
-
If you don’t have symptoms, another test isn’t necessary.
-
-
Before attending events or meeting high-risk people: Testing can help prevent spreading the virus.
COVID-19 tests use samples taken from your nose, throat, or saliva.
Types of COVID-19 Tests
-
Molecular tests (PCR or NAAT)
-
Detect the genetic material of the virus.
-
Highly accurate and usually performed by healthcare professionals, though some at-home options exist.
-
Results may take longer since samples are typically processed in a laboratory.
-
-
Antigen tests (rapid tests)
-
Detect viral proteins (antigens).
-
Provide results quickly and are often used at home.
-
Reliable for detecting infection when symptoms are present but less accurate than PCR tests, especially in people without symptoms.
-
If the result is negative, repeat the test after 48 hours for confirmation.
-
Understanding Test Results
-
Positive result (PCR or antigen):
You almost certainly have COVID-19. No additional test is needed. -
Negative PCR result:
You most likely do not have COVID-19. -
Negative antigen result:
The FDA recommends repeating the test two days later for a more accurate diagnosis.
If you test positive, contact your healthcare professional right away to discuss treatment options.
Preventing the Spread While Sick
To avoid infecting others:
-
Stay home and isolate from others until your symptoms improve.
-
If you have a weakened immune system, you may need to isolate longer—follow your doctor’s advice.
-
If you must be around others, wear a face mask and avoid sharing items such as cups or towels.
-
Use a separate bathroom and bedroom, if possible.
-
Improve airflow in your home by opening windows or using air purifiers.
You can end isolation when:
-
You feel better,
-
You have been fever-free for 24 hours without medication, and
-
Your symptoms are improving.
If your fever returns or symptoms worsen, resume isolation until you meet the above criteria again.
For five days after isolation, continue to:
-
Wear a mask,
-
Wash your hands frequently,
-
Keep physical distance,
-
Take a test if needed, and
-
Ensure good ventilation indoors.
Treatment
Most people recover from COVID-19 with rest, fluids, and symptom management.
Over-the-counter (OTC) medications may help:
-
Fever reducers
-
Pain relievers such as ibuprofen (Advil, Motrin IB) or acetaminophen (Tylenol)
-
Cough syrup or cough medicine
Antiviral medicines for high-risk individuals:
If you are at high risk of severe illness, your healthcare provider may prescribe:
-
Nirmatrelvir-ritonavir (Paxlovid) – oral pills
-
Remdesivir (Veklury) – given through an IV
-
Molnupiravir (Lagevrio) – oral pills
If your condition worsens, hospitalization may be required.
Treatment for Severe COVID-19
People hospitalized for COVID-19 receive care based on their immune response and oxygen needs.
-
Oxygen therapy: Given through nasal tubes or, in severe cases, mechanical ventilation.
-
Extracorporeal membrane oxygenation (ECMO): A machine temporarily replaces heart and lung function in critical cases.
Medications for severe COVID-19 may include:
-
Remdesivir (antiviral)
-
Baricitinib (Olumiant) – oral pill that reduces inflammation
-
Tocilizumab (Actemra) – IV medicine that targets inflammation
-
Dexamethasone – corticosteroid given orally or via IV to reduce lung inflammation
Convalescent plasma therapy may also be considered for patients with weakened immune systems. This treatment uses antibody-rich plasma donated by recovered COVID-19 patients to help fight the infection.
Advertisement