Overview
Diagnosis
Cushing syndrome can be caused by long-term use of glucocorticoid medicines or by the body producing too much cortisol. Diagnosing this condition can be complex because many of its symptoms resemble those of other health problems. An endocrinologist — a specialist in hormone-related disorders — usually performs the diagnosis.
Physical exam
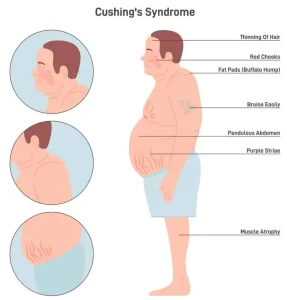
The endocrinologist checks for classic signs of Cushing syndrome such as:
-
Round, full face (moon face)
-
Hump on the upper back or neck (buffalo hump)
-
Thin, fragile skin that bruises easily
-
Purple stretch marks (striae)
Blood and urine tests
-
24-hour urine cortisol test: Measures cortisol levels in urine collected over a full day to check for excessive hormone production.
-
Blood tests: Measure cortisol and ACTH (adrenocorticotropic hormone) levels to determine if the body is making too much cortisol.
-
Stimulation or suppression tests: These evaluate how cortisol levels change after taking specific hormone medicines.
Saliva test
Cortisol levels normally decrease in the evening. A late-night saliva test can show if cortisol remains high, which is a key sign of Cushing syndrome.
Imaging tests
-
CT (computerized tomography) scan or MRI (magnetic resonance imaging) may be used to look for tumors in the pituitary or adrenal glands that could be causing excess cortisol.
Inferior petrosal sinus sampling
If imaging tests do not clearly identify the cause, this specialized procedure helps determine whether excess ACTH is coming from the pituitary gland or another part of the body.
-
A catheter is inserted through a vein in the groin or neck to collect blood from veins near the pituitary gland (called inferior petrosal sinuses).
-
Blood is also taken from the forearm for comparison.
-
After a stimulating medicine is given, ACTH levels are measured in both samples.
-
Higher ACTH in the sinus sample → tumor in the pituitary gland.
-
Similar ACTH levels → ACTH-producing tumor elsewhere in the body.
-
These tests help confirm Cushing syndrome and rule out other conditions with similar symptoms, such as polycystic ovary syndrome (PCOS), depression, alcoholism, or eating disorders.
Treatment
The goal of treatment is to reduce cortisol levels to normal. The best approach depends on the cause of the syndrome.
Reducing glucocorticoid use
If caused by long-term glucocorticoid medication, the dose may be gradually lowered under medical supervision.
⚠️ Do not stop glucocorticoids suddenly, as this can cause dangerously low cortisol levels. The tapering process allows your body to begin producing cortisol naturally again.
Surgery
If a tumor is causing excess cortisol, surgical removal is the preferred treatment.
-
Pituitary tumors: Removed by a neurosurgeon through the nose (transsphenoidal surgery).
-
Adrenal tumors: Removed using traditional or minimally invasive surgery.
-
Other ACTH-producing tumors: May require additional procedures.
If the tumor can’t be removed or found, both adrenal glands may be removed (bilateral adrenalectomy) to stop cortisol production. In that case, lifelong hormone replacement for cortisol and aldosterone is required.
Radiation therapy
Used when pituitary tumors cannot be fully removed or surgery is not possible.
-
May involve small doses over several weeks or a single high dose.
-
Modern radiation planning helps protect nearby healthy tissue.
Medications
When surgery or radiation isn’t effective or possible, medicines can help control cortisol levels:
-
Ketoconazole, osilodrostat (Isturisa), mitotane (Lysodren), levoketoconazole (Recorlev), metyrapone (Metopirone) — reduce cortisol production at the adrenal gland.
-
Mifepristone (Korlym, Mifeprex) — blocks cortisol’s effects on tissues; used in people with Cushing syndrome and type 2 diabetes or high blood sugar.
-
Pasireotide (Signifor) — reduces ACTH release from pituitary tumors.
Possible side effects include:
-
Fatigue
-
Nausea or vomiting
-
Headaches
-
High blood pressure
-
Low potassium
-
Muscle pain or swelling
-
In rare cases, liver or nervous system problems
If treatment causes low levels of other hormones, your healthcare provider may recommend hormone replacement therapy.
Advertisement