Overview
Diagnosis
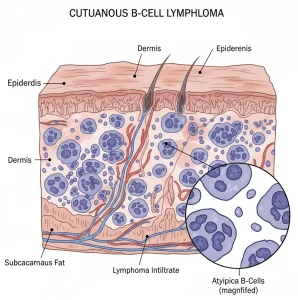
Cutaneous B-cell lymphoma is diagnosed through a combination of physical examination, biopsies, blood tests, and imaging studies to confirm the presence of lymphoma cells and determine how far the disease has spread.
Tests and procedures used for diagnosis include:
-
Physical exam:
Your healthcare professional carefully examines the skin to check for lumps, plaques, or lesions and looks for other signs that might help confirm the diagnosis. -
Skin biopsy:
A biopsy involves removing a small piece of affected skin for laboratory testing. Under a microscope, specialists look for B-cell lymphoma cells to confirm the diagnosis. -
Blood tests:
A blood sample may be analyzed to detect lymphoma cells or other abnormalities related to the disease. -
Bone marrow biopsy:
A bone marrow sample is tested to see if lymphoma cells have spread beyond the skin. -
Imaging tests:
Imaging helps assess whether the cancer has spread to other parts of the body.
Examples include:-
CT (Computerized Tomography) scan
-
PET (Positron Emission Tomography) scan
-
Treatment
Treatment for cutaneous B-cell lymphoma depends on the specific subtype, the extent of disease, and how quickly it is growing.
Treatment options may include:
-
Radiation therapy:
Uses high-energy beams, such as X-rays or protons, to destroy cancer cells.-
Can be used alone to treat localized lymphoma.
-
Sometimes given after surgery to eliminate any remaining cancer cells.
-
-
Surgery to remove the cancer:
The cancerous area and some surrounding healthy tissue may be surgically removed.-
Best suited for patients with one or a few localized lesions.
-
Surgery alone may be enough in some cases, though additional treatments may follow.
-
-
Injecting medicine into the cancer:
In cases of slow-growing cutaneous lymphoma, steroid medicines or other agents may be injected directly into the cancer to shrink it. -
Chemotherapy:
Uses strong anti-cancer medicines to kill lymphoma cells.-
May be applied to the skin for local control.
-
May also be given through a vein (systemic chemotherapy) if the disease is advanced or rapidly progressing.
-
-
Targeted therapy:
Focuses on specific molecules in cancer cells that help them grow and survive.-
Can be injected directly into the lymphoma or administered intravenously.
-
Helps block cancer cell growth and cause the cells to die.
-
Advertisement