Overview
Diagnosis
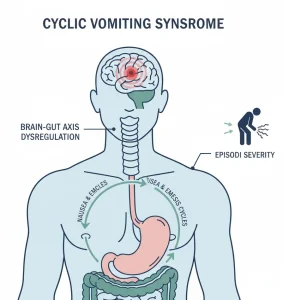
Cyclic vomiting syndrome (CVS) can be difficult to diagnose because there’s no specific test to confirm it, and vomiting can occur due to many other health conditions.
A healthcare professional usually begins by reviewing your or your child’s medical history and performing a physical examination. The provider may also ask detailed questions about the pattern and triggers of vomiting episodes, including their frequency, duration, and severity.
To rule out other possible causes, the following tests may be recommended:
-
Imaging studies:
Tests such as endoscopy, ultrasound, or a CT scan help check for blockages or abnormalities in the digestive system. -
Motility tests:
These tests evaluate how food moves through the digestive tract and help detect digestive disorders that affect movement or coordination. -
Laboratory tests:
Used to check for thyroid problems, metabolic conditions, or other disorders that may mimic CVS symptoms.
Treatment
There is no cure for cyclic vomiting syndrome (CVS), but treatment aims to manage symptoms, prevent episodes, and reduce their intensity. Many children tend to outgrow CVS as they reach adulthood.
During an active episode, treatment focuses on symptom control, which may include:
-
Antinausea medicines to control vomiting.
-
Pain-relieving medicines to ease abdominal pain.
-
Acid-suppressing medicines to protect the stomach lining.
-
Antidepressants or antiseizure medicines to help stabilize body responses and reduce the frequency of episodes.
-
Migraine medicines, since CVS can sometimes be linked to migraine-type symptoms and may respond to similar treatments.
If vomiting is severe, intravenous (IV) fluids may be required to prevent dehydration and electrolyte imbalance.
The treatment plan depends on:
-
The severity and duration of each episode.
-
The frequency of episodes.
-
Any related complications, such as dehydration or nutritional deficiencies.
Advertisement