Overview
Diagnosis
Diagnosing dementia involves identifying patterns of memory loss, cognitive decline, and changes in daily functioning. A healthcare professional reviews medical history, performs exams, and may use several tests to determine the cause.
Key diagnostic steps include:
-
Cognitive and neuropsychological tests – These measure memory, reasoning, language, attention, and judgment skills to assess cognitive decline.
-
Neurological evaluation – Movement, reflexes, balance, coordination, and sensory response are checked to identify neurological causes.
-
Brain scans –
-
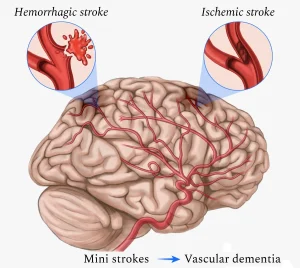
CT or MRI: Used to detect stroke, bleeding, tumors, or fluid buildup (hydrocephalus).
-
PET scans: Identify brain activity patterns and detect amyloid or tau proteins, which are signs of Alzheimer’s disease.
-
-
Laboratory tests – Blood tests check for conditions such as thyroid disorders or vitamin B-12 deficiency that can affect brain function. In some cases, spinal fluid analysis is done to detect infection or disease markers.
-
Psychiatric exam – A mental health evaluation helps rule out depression or other psychiatric conditions that may mimic dementia symptoms.
Treatment
While most types of dementia cannot be cured, treatment focuses on managing symptoms, improving quality of life, and slowing disease progression.
Medications
-
Cholinesterase inhibitors – Improve memory and thinking by increasing levels of brain chemicals. Common drugs include donepezil, rivastigmine, and galantamine. These may also help in vascular, Parkinson’s, or Lewy body dementia.
-
Side effects: nausea, vomiting, diarrhea, slowed heart rate, fainting, and sleep issues.
-
-
Memantine (Namenda) – Regulates glutamate activity, supporting memory and learning functions. Often used alongside a cholinesterase inhibitor. Common side effect: dizziness.
-
Other medicines – Used to manage depression, sleep issues, hallucinations, agitation, or stiffness.
-
Lecanemab (Leqembi) and Donanemab (Kisunla) – FDA-approved for mild Alzheimer’s and mild cognitive impairment. They reduce amyloid plaque buildup and slow cognitive decline.
-
Side effects: flu-like symptoms, nausea, vomiting, dizziness, and rare but serious brain swelling or bleeding.
-
Genetic testing for the APOE e4 gene and brain MRI scans are recommended before treatment due to potential risks.
-
Therapies
-
Occupational therapy – Helps create a safe home environment, reduce fall risks, and teach coping skills for daily living.
-
Environmental modifications – Reducing clutter, limiting noise, and removing dangerous items like knives or car keys can enhance safety and focus.
-
Simplified routines – Breaking tasks into smaller steps and maintaining consistent schedules reduces confusion and frustration.
Managing dementia involves ongoing support, clear communication, and adjustments to maintain independence and safety for as long as possible.
Advertisement