Overview
Diagnosis
Diabetic retinopathy is often diagnosed with a dilated eye exam. During this exam, an eye care professional places drops in your eyes to widen the pupils. This allows a clearer view of the internal structures of the eyes. The drops may cause blurred near vision for several hours after the test.
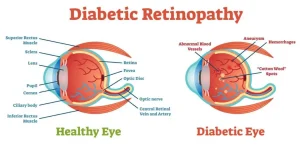
During the eye exam, the specialist looks for abnormalities in both the internal and external parts of the eyes, such as leaking blood vessels, swelling, or new abnormal vessel growth.
Other important tests used to confirm and assess the severity of diabetic retinopathy include:
-
Optical coherence tomography (OCT): This imaging test provides detailed cross-sectional views of the retina. It shows retinal thickness and helps detect fluid accumulation within the retinal layers. OCT is also used over time to monitor the effectiveness of treatment.
-
Fluorescein angiography: After dilating the pupils, a dye is injected into a vein in the arm. As the dye circulates through the blood vessels of the eyes, photographs are taken to identify areas where blood vessels are leaking, blocked, or damaged.
Treatment
Treatment for diabetic retinopathy depends on the stage of the disease and the type of damage seen in the retina. The goal is to slow or stop progression and preserve vision.
Early Diabetic Retinopathy
In the early stages, called nonproliferative diabetic retinopathy, treatment might not be needed immediately. Regular monitoring and improved diabetes management are key. Maintaining stable blood sugar levels can significantly slow the disease’s progression and prevent vision loss.
Your eye care professional may schedule follow-up exams to closely track any changes in the retina.
Advanced Diabetic Retinopathy
When the condition advances to proliferative diabetic retinopathy or macular edema develops, active treatment becomes necessary. A retina specialist determines the best therapy depending on the severity and location of the retinal changes.
Common treatment options include:
-
Eye injections:
Medications called vascular endothelial growth factor (VEGF) inhibitors are injected into the eye’s vitreous cavity. These drugs prevent abnormal blood vessel growth and reduce fluid buildup.
Approved VEGF inhibitors include ranibizumab (Lucentis), aflibercept (Eylea), and faricimab (Vabysmo). Bevacizumab (Avastin) is also widely used off-label for diabetic macular edema.
Injections are performed under local anesthesia and may cause mild discomfort such as burning, tearing, or soreness for up to 24 hours. Side effects can include temporary pressure increase inside the eye or, rarely, infection.
Repeat injections are often required, and they may be combined with laser therapy for better results. -
Laser therapy (laser photocoagulation):
This procedure uses focused laser light to seal or shrink abnormal retinal blood vessels. It helps prevent leakage and reduces the growth of new, fragile vessels.
Laser therapy is usually done in an outpatient setting, often requiring more than one session. Temporary blurry vision or minor loss of side or night vision can occur after treatment. -
Vitrectomy:
In advanced cases, a surgical procedure called vitrectomy may be needed. The surgeon removes blood or scar tissue from the vitreous cavity using tiny instruments inserted through the white part of the eye. This helps clear vision and repair retinal detachment if present.
Vitrectomy is performed in a hospital or surgery center under local or general anesthesia.
Ongoing Care
Even after treatment, diabetic retinopathy requires regular follow-up. Because diabetes is a long-term condition, continued damage to the retina can still occur. Regular eye exams help detect new changes early, allowing timely intervention to preserve vision.
Advertisement