Overview
Diagnosis
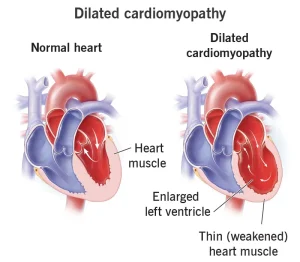
To diagnose dilated cardiomyopathy, a healthcare provider conducts a physical examination and reviews the patient’s personal and family medical history. Using a stethoscope, the provider listens to the heart and lungs for signs of abnormal sounds or fluid buildup. Referral to a cardiologist is common for further evaluation.
Tests
Several diagnostic tests are used to confirm dilated cardiomyopathy and assess heart function:
-
Echocardiogram: The primary test for diagnosing dilated cardiomyopathy. It uses sound waves to produce moving images of the heart, showing how blood flows through the chambers and valves, and whether the left ventricle is enlarged.
-
Blood tests: These tests detect infections, metabolic issues, or diseases such as diabetes or hemochromatosis that may contribute to cardiomyopathy.
-
Chest X-ray: Provides an image of the heart and lungs, showing the size of the heart and whether fluid is present in or around the lungs.
-
Electrocardiogram (ECG or EKG): Records the heart’s electrical activity to reveal rhythm abnormalities, heart rate, and potential blood flow issues.
-
Holter monitor: A portable ECG worn for 24 hours or more to record continuous heart activity during daily routines.
-
Exercise stress test: Evaluates how the heart responds to physical activity, often performed on a treadmill or stationary bike. Medications may be used if exercise isn’t possible.
-
Cardiac CT or MRI scan: Produces detailed images showing the size, structure, and pumping function of the heart’s chambers.
-
Cardiac catheterization: A procedure in which thin tubes are inserted into blood vessels to reach the heart. Dye is injected for X-ray imaging, and a tissue sample (biopsy) may be taken to assess heart muscle damage.
-
Genetic screening or counseling: Since dilated cardiomyopathy can be inherited, genetic testing may be recommended for patients and close family members.
Treatment
The treatment of dilated cardiomyopathy focuses on relieving symptoms, improving heart function, and preventing further damage. It may include medications, lifestyle changes, or surgical procedures.
Medications
A combination of medications helps the heart pump more efficiently, control rhythm, lower blood pressure, and prevent complications such as blood clots or fluid buildup.
Commonly used drugs include:
-
Blood pressure medications: Beta-blockers, ACE inhibitors, and angiotensin II receptor blockers (ARBs) improve blood flow and reduce heart strain.
-
Sacubitril/valsartan (Entresto): Combines two types of medication to enhance heart pumping efficiency, particularly for chronic heart failure.
-
Water pills (diuretics): Remove excess fluid and salt, reducing swelling and easing breathing difficulties.
-
Digoxin (Lanoxin): Strengthens heart contractions and slows the heartbeat, helping relieve heart failure symptoms.
-
Ivabradine (Corlanor): Occasionally used to manage heart failure by lowering the heart rate.
-
Blood-thinners (anticoagulants): Prevent blood clots that can lead to stroke or other complications.
Surgeries or Other Procedures
When medications are not enough, surgical procedures or medical devices may be required to regulate heart rhythm or improve blood circulation.
Types of devices and procedures include:
-
Biventricular pacemaker: Helps both lower chambers of the heart beat in sync, improving overall heart function in patients with heart failure.
-
Implantable cardioverter-defibrillator (ICD): Monitors heart rhythm and delivers an electric shock if life-threatening arrhythmias occur.
-
Left ventricular assist device (LVAD): A mechanical pump that helps the heart circulate blood, used either temporarily before a transplant or as long-term therapy.
If other treatments fail, a heart transplant may be the final option for patients with advanced dilated cardiomyopathy.
Advertisement