Overview
Diagnosis
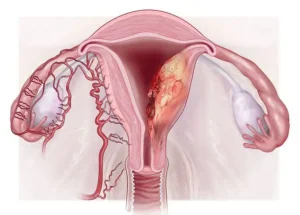
Diagnosing endometrial cancer involves a series of examinations and imaging tests to identify cancerous changes in the lining of the uterus.
Tests and procedures used to diagnose endometrial cancer include:
-
Pelvic exam: A physical examination of the reproductive organs. The healthcare professional inspects the outer genital area and uses a speculum to view the vaginal canal and cervix. The uterus and ovaries are felt through the abdominal wall to detect abnormalities.
-
Imaging tests: These create detailed pictures of internal organs.
-
Transvaginal ultrasound: A wandlike device (transducer) is inserted into the vagina to produce images of the uterus. It helps assess the thickness and texture of the endometrium and detect possible tumors or irregularities.
-
Other imaging methods such as MRI or CT scans may be used to gather more information about the cancer’s location and spread.
-
-
Hysteroscopy: A thin, flexible tube with a light and camera, called a hysteroscope, is inserted through the vagina into the uterus. This allows the healthcare professional to visually inspect the uterine lining for abnormal growths or cancer signs.
-
Endometrial biopsy: A small sample of tissue is removed from the uterine lining and sent to a laboratory to check for cancer cells. This is usually performed in a clinic.
-
Dilation and curettage (D&C): If biopsy samples are insufficient or results are unclear, this surgical procedure is performed. It involves scraping tissue from the uterine lining for microscopic examination.
If cancer is confirmed, patients are often referred to a gynecologic oncologist, a specialist in cancers of the reproductive system.
Staging endometrial cancer
After diagnosis, additional tests determine how far the cancer has spread, known as staging. These may include:
-
Chest X-ray
-
CT scan
-
Blood tests
-
PET scan
Staging helps classify cancer from Stage 1 to Stage 4, where Stage 1 is limited to the uterus and Stage 4 indicates spread to nearby or distant organs such as the bladder or other body parts.
Treatment
Treatment for endometrial cancer typically begins with surgery and may include radiation, chemotherapy, hormone therapy, or newer targeted treatments. The plan depends on the stage of the cancer, overall health, and personal preferences.
Surgery
-
The main treatment is hysterectomy, a procedure to remove the uterus.
-
Most patients also undergo salpingo-oophorectomy, which removes the fallopian tubes and ovaries.
-
During surgery, nearby lymph nodes may be removed for testing to determine whether cancer has spread.
-
This procedure ends the ability to become pregnant and triggers menopause if it hasn’t already occurred.
Radiation therapy
-
Uses high-energy beams, such as X-rays or protons, to destroy cancer cells.
-
Can be done before surgery to shrink tumors or after surgery to kill any remaining cancer cells.
-
May also be used alone if surgery isn’t possible.
-
Types include:
-
External beam radiation therapy: Radiation is directed at the uterus from outside the body.
-
Brachytherapy: A radiation-filled device is placed inside the vagina for a short time.
-
Chemotherapy
-
Involves strong medicines that kill cancer cells throughout the body.
-
Can be given after surgery to reduce recurrence risk or before surgery to shrink tumors.
-
Typically used for advanced or recurrent endometrial cancer.
Hormone therapy
-
Reduces hormone levels to slow or stop cancer growth.
-
Used in advanced or metastatic cases, especially when cancer cells rely on hormones like estrogen.
Targeted therapy
-
Focuses on specific molecules in cancer cells that help them grow.
-
Often combined with chemotherapy for advanced or resistant cancer types.
Immunotherapy
-
Helps the immune system identify and attack cancer cells.
-
Used for advanced or recurrent endometrial cancers that don’t respond to standard treatments.
Palliative care
-
Provides symptom relief and emotional support during treatment.
-
A multidisciplinary team focuses on improving quality of life through pain management and psychological care.
-
Can be combined with active cancer treatments and has been shown to help patients feel better and live longer.
Advertisement