Overview
Diagnosis
To diagnose gynecomastia, your healthcare provider begins with a detailed medical history and physical examination. You’ll likely be asked about your symptoms, medications, and any underlying health issues. During the exam, your provider will check your breast tissue, stomach area, and genitals to identify any abnormalities or hormone-related signs.
Tests
Your healthcare team may order several tests to find the cause of gynecomastia or rule out other possible conditions:
-
Blood tests: Help identify hormonal imbalances or medical conditions that may cause gynecomastia.
-
Mammogram: An X-ray of the breast to detect abnormal tissue growth or signs of breast cancer.
-
CT scan: A detailed imaging test that takes X-rays from different angles to identify tumors or gland abnormalities.
-
MRI scan: Uses magnetic fields and radio waves to provide detailed images of soft tissue structures, including breast tissue.
-
Testicular ultrasound: Uses sound waves to check the testicles and surrounding tissue for tumors or abnormalities affecting hormone levels.
-
Tissue biopsy: Removes a small piece of breast tissue for lab testing to rule out breast cancer or other diseases.
Conditions that cause similar symptoms
Your healthcare team will confirm that the breast enlargement is due to gynecomastia and not another condition. Possible look-alike conditions include:
-
Fatty breast tissue (Pseudogynecomastia): Common in people with obesity, where breast fat increases but no glandular growth occurs. No further testing is typically needed.
-
Breast cancer: Rare in men but possible. A hard, firm lump or enlargement of only one breast may suggest male breast cancer.
-
Mastitis: Inflammation of breast tissue, sometimes with infection, causing swelling and tenderness.
-
Lipoma: A noncancerous, slow-growing lump made up of fatty tissue.
Treatment
Gynecomastia often resolves without medical treatment, especially when it’s related to puberty or temporary hormonal changes. However, treatment may be required if the condition persists, causes pain, or leads to emotional distress.
Observation and lifestyle management
-
In teenagers, gynecomastia due to puberty-related hormonal changes often goes away within two years.
-
Regular checkups every 3–6 months may be recommended to monitor progress.
-
If a medication is the cause, your doctor might stop or replace it with a different one.
Medications
Certain medicines used to treat other conditions may help reduce gynecomastia in adults:
-
Tamoxifen (Soltamox) – a selective estrogen receptor modulator.
-
Raloxifene (Evista) – also used for osteoporosis and hormone-related conditions.
-
Aromatase inhibitors (Anastrozole, Arimidex) – block estrogen production.
These drugs are FDA-approved for other uses but not specifically approved to treat gynecomastia.
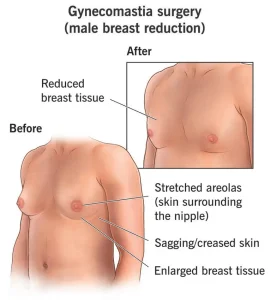
Surgery to remove excess breast tissue
If gynecomastia doesn’t resolve with observation or medication and causes significant discomfort or embarrassment, surgical options include:
-
Liposuction: Removes excess fat tissue from the breast but leaves glandular tissue intact.
-
Mastectomy: Removes glandular breast tissue through small incisions for quicker recovery.
-
In some cases, liposuction and mastectomy are combined for best results.
-
Surgery provides permanent results and is often considered when gynecomastia persists despite medical management.
Advertisement