Overview
Diagnosis
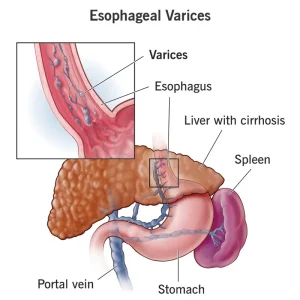
Diagnosis of esophageal varices usually begins after a person is diagnosed with cirrhosis or other conditions that increase pressure in the portal vein (portal hypertension). The goal of diagnosis is to detect swollen veins in the esophagus early to prevent bleeding.
Upper endoscopy
An upper endoscopy is the preferred and most accurate test for detecting esophageal varices. A flexible tube with a small camera at the tip is inserted through the mouth to examine the esophagus, stomach, and upper part of the small intestine (duodenum).
During the test, a healthcare professional looks for enlarged veins and may identify red streaks or spots, which indicate a higher risk of bleeding. If varices are found, treatment such as band ligation can be performed immediately during the same procedure.
Imaging tests
Imaging can help suggest the presence of varices and assess liver scarring or portal hypertension:
-
CT scan or Doppler ultrasound of the abdomen can reveal changes in the splenic and portal veins.
-
Transient elastography measures liver stiffness, helping determine if cirrhosis or portal hypertension is present.
These tests are noninvasive but are less precise than endoscopy for detecting bleeding risk.
Treatment
The primary goal in treating esophageal varices is to prevent bleeding, which can be life-threatening. If bleeding has already occurred, emergency treatment is required to stop it and prevent recurrence.
Treatment to prevent bleeding
-
Medicines to lower portal vein pressure:
Beta blockers such as propranolol (Inderal, Innopran XL) and nadolol help reduce pressure in the portal vein, lowering the risk of rupture. -
Endoscopic band ligation:
During endoscopy, elastic bands are placed around the swollen veins to block blood flow. This prevents rupture and future bleeding. The procedure may cause mild complications like esophageal scarring or temporary discomfort.
Treatment for active bleeding
If bleeding occurs, immediate medical attention is crucial. Treatments include:
-
Endoscopic band ligation: Elastic bands are used to tie off bleeding veins.
-
Medicines to reduce blood flow to the portal vein: Drugs like octreotide (Sandostatin) or vasopressin (Vasostrict) decrease blood flow and help control bleeding. Treatment continues for up to 5 days after a bleeding episode.
-
TIPS (Transjugular Intrahepatic Portosystemic Shunt):
If bleeding doesn’t stop with medicine or banding, a TIPS procedure may be performed. A small channel is created between the portal and hepatic veins, allowing blood to bypass the scarred liver and reducing pressure.
However, TIPS carries risks such as liver failure or mental confusion (hepatic encephalopathy) due to toxins bypassing the liver. It’s mainly used when other treatments fail or as a bridge to liver transplantation. -
Balloon tamponade:
In emergencies, a balloon may be inflated in the esophagus to apply pressure and temporarily stop bleeding. This is a short-term measure (less than 24 hours) before definitive treatment like TIPS. It carries risks such as esophageal rupture and bleeding recurrence after deflation. -
Blood transfusion and clotting factors:
Used to replace lost blood and restore normal clotting ability. -
Antibiotics:
Given to prevent infections, which are common in people with bleeding varices. -
Liver transplant:
In severe cases or recurrent bleeding, a liver transplant is the best long-term solution.
Rebleeding
People who have experienced variceal bleeding have a high risk of rebleeding.
To prevent recurrence:
-
Beta blockers and endoscopic band ligation are recommended together.
-
Follow-up endoscopies are scheduled at regular intervals to monitor and treat remaining or new varices.
Potential Future Treatments
New and experimental approaches are being studied to improve outcomes:
-
Hemostatic powder: Sprayed through a catheter during endoscopy, this powder sticks to varices and stops bleeding quickly.
-
Self-expanding metal stents (SEMS): Placed during endoscopy, these stents put pressure on bleeding veins to stop bleeding. They are temporary (up to 7 days) and used when other measures fail. However, they may damage tissue or migrate, so they are still considered experimental.
Advertisement