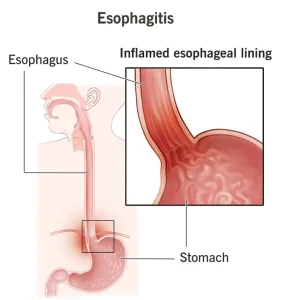
Overview
Diagnosis
Diagnosis of esophagitis involves several steps to identify the cause and severity of inflammation in the esophagus. Your healthcare professional or specialist will begin by asking about your symptoms and performing a physical exam. Depending on your condition, one or more diagnostic tests may be required.
Endoscopy
Endoscopy is a primary test used to examine the digestive system. A healthcare professional inserts a long, thin, flexible tube with a tiny camera, called an endoscope, through the throat into the esophagus. This allows direct visualization of any inflammation, ulcers, or narrowing. During the procedure, small tissue samples may be taken for testing, known as a biopsy. The esophagus may appear differently depending on the type of esophagitis, such as reflux, eosinophilic, or medicine-induced. Sedation is usually provided to help you relax during the procedure.
Esophageal capsule test
This test is performed in the healthcare provider’s office. It involves swallowing a capsule attached to a thin string. Once in the stomach, the capsule dissolves and releases a small sponge. The sponge is gently pulled out through the mouth, collecting tissue samples from the esophagus along the way. These samples help determine the level of inflammation without requiring an endoscopy.
Barium X-ray
A barium X-ray, also known as an upper GI series, involves drinking a barium-containing solution or swallowing a pill. Barium coats the esophagus and stomach lining, making them visible on X-ray images. The images can help identify narrowing, ulcers, hernias, or tumors that may be causing symptoms.
Laboratory tests
Tissue samples taken during endoscopy are sent to a laboratory for further testing. These tests help to:
-
Detect infections caused by bacteria, viruses, or fungi
-
Identify allergy-related white blood cells called eosinophils
-
Detect abnormal or precancerous cells that may increase cancer risk
Treatment
Treatment for esophagitis aims to relieve symptoms, heal inflammation, manage complications, and address the underlying cause. The approach varies based on the specific type of esophagitis.
Reflux esophagitis
Treatment for reflux esophagitis focuses on reducing acid production and preventing acid reflux into the esophagus.
-
Over-the-counter medicines such as antacids (Maalox, Mylanta), H-2-receptor blockers (cimetidine, Tagamet HB), and proton pump inhibitors (lansoprazole, Prevacid 24 HR; omeprazole, Prilosec OTC) are often used.
-
Prescription-strength medicines may be required for more severe cases.
-
Surgery such as fundoplication may be performed if medications do not provide relief. This procedure strengthens the valve between the stomach and esophagus to prevent acid backflow.
Eosinophilic esophagitis
Eosinophilic esophagitis is treated by avoiding allergens and reducing inflammation.
-
Proton pump inhibitors are usually prescribed first, such as esomeprazole (Nexium) or pantoprazole (Protonix).
-
Swallowed steroids like budesonide (Eohilia) or fluticasone help decrease inflammation directly in the esophagus.
-
Dietary changes through elimination or elemental diets may help identify and remove triggering foods under medical supervision.
-
Monoclonal antibodies such as dupilumab (Dupixent) can help reduce inflammation in patients aged 12 and older when other treatments are ineffective.
Medicine-induced esophagitis
This condition is treated by modifying how and what medications are taken.
-
Switching to an alternative medication or a liquid form may reduce irritation.
-
Pills should be taken with a full glass of water and without lying down for at least 30 minutes afterward.
-
People with fluid restrictions, such as those with kidney disease, should follow their healthcare provider’s advice.
Infectious esophagitis
Treatment focuses on eliminating the infection responsible for inflammation.
-
Antiviral, antibacterial, or antifungal medications are prescribed depending on the infection type.
Treating complications
In cases where the esophagus becomes very narrow or food gets stuck, a gastroenterologist may perform a procedure called esophageal dilation. This involves using specialized medical tools to gently widen the esophagus.
-
Some tools use a tapered tip that gradually expands the passage.
-
Others use a balloon that inflates once inside the esophagus to stretch the narrowed area.
This procedure helps restore normal swallowing and prevent food obstruction.
Advertisement