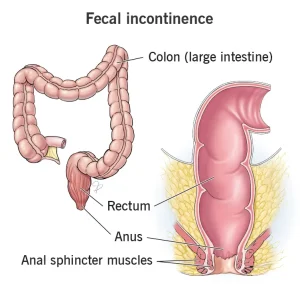
Overview
Diagnosis
Your healthcare professional will ask questions about your symptoms, diet, and medical history to determine the cause of fecal incontinence. A detailed medical examination is usually done to assess muscle and nerve function in the anal and rectal area.
Anal and rectal exam
Your healthcare professional will examine the area around the anus to check muscle reflexes and identify any irregular tissues. During the exam, a gloved finger may be gently inserted into the anus to detect problems with muscles, tissues, or large, hard stool in the rectum.
Neurological exam
A neurological exam evaluates the overall health of the nervous system, including reflexes, coordination, balance, and sensation. This helps identify any nerve-related causes of fecal incontinence.
Tests of rectal and anal function
These tests assess how well the rectum and anus function during bowel movements:
-
Anorectal manometry: A narrow, flexible device is inserted into the anus and rectum to measure muscle strength, nerve response, and rectal expansion.
-
Balloon expulsion test: A small balloon filled with water is placed in the rectum. You are then asked to expel it to assess how effectively you can empty stool.
Imaging tests
Imaging studies help visualize the rectum, colon, and surrounding structures to identify abnormalities.
-
Endoscopy: A flexible tube with a camera examines the rectum and colon for inflammation, cancer, or other tissue irregularities.
-
Endoscopic ultrasound: Combines endoscopy and ultrasound to provide detailed images of rectal and colon tissues.
-
Defecography: Uses X-ray or MRI imaging while you pass stool to assess the physical and functional condition of the rectum and anus.
-
Anorectal MRI: Provides detailed information about the muscles of the anus and rectum.
Treatment
The main goal of treatment is to manage conditions that cause or worsen fecal incontinence and improve rectal and anal muscle function.
Diet and lifestyle changes
The first step involves making healthy changes to diet and daily habits:
-
Add high-fiber foods gradually to your diet, such as:
-
Vegetables and fruits
-
Whole-grain foods
-
Beans and legumes
-
-
Avoid foods that may cause diarrhea, including:
-
Caffeinated, alcoholic, or artificially sweetened drinks
-
Fatty or dairy-heavy foods
-
Foods high in fructose, such as apples, peaches, and pears
-
Spicy foods
-
Other healthy lifestyle changes include exercising regularly, staying hydrated, maintaining a healthy weight, and quitting smoking.
Medicines
Your healthcare professional may recommend medications or supplements depending on the cause:
-
Anti-diarrheal drugs: Loperamide (Imodium A-D), diphenoxylate with atropine (Lomotil), or bismuth subsalicylate (Pepto-Bismol).
-
Fiber supplements: Methylcellulose (Citrucel) or psyllium (Metamucil, Konsyl) to treat constipation-related incontinence.
-
Laxatives: Magnesium hydroxide, polyethylene glycol (MiraLAX), or bisacodyl (Dulcolax) to relieve constipation.
Exercise and training
Specific exercises and training can strengthen the anal, rectal, and pelvic floor muscles, improving control over bowel movements.
-
Kegel exercises: Strengthen the muscles used to stop urination or gas. Contract for three seconds, relax for three seconds, and repeat 10–15 times. Gradually increase the hold time as strength improves.
-
Biofeedback training: Uses sensors and visual or auditory feedback to help you strengthen muscles and recognize sensations that signal when stool is ready to pass.
-
Bowel training: Encourages regular bowel movements by scheduling toilet visits at consistent times, such as after meals.
Other treatments
When conservative treatments don’t work, other options may be considered:
-
Bulking agents: Injections that thicken the anal walls to reduce leakage.
-
Sacral nerve stimulation: A small device implanted under the skin sends mild electrical impulses to the sacral nerves, improving muscle control.
-
Inserted devices: Anal plugs or vaginal inserts can help block or control leakage.
Surgery
Surgery may be recommended when other treatments are not effective or when an underlying structural problem exists.
-
Surgery for underlying issues: Procedures to correct rectal prolapse, rectocele, or hemorrhoids.
-
Sphincteroplasty: Repairs a damaged or weakened anal sphincter, often caused by childbirth. The muscle edges are stitched together to strengthen the sphincter.
-
Colostomy (bowel diversion): Creates an opening in the abdomen to divert stool into a special bag. This is considered only when all other treatments fail.
Advertisement