Overview
Diagnosis
If you’ve been unable to conceive after trying for a reasonable period, consult your doctor for a fertility evaluation. Both partners are usually assessed to identify possible causes. Your doctor will review your medical history, perform a physical exam, and recommend appropriate tests.
Fertility Tests for Women
Ovulation testing
An over-the-counter ovulation prediction kit detects the luteinizing hormone (LH) surge that occurs just before ovulation. A blood test measuring progesterone — the hormone produced after ovulation — can confirm whether ovulation is occurring. Other hormone levels, such as prolactin, may also be checked.
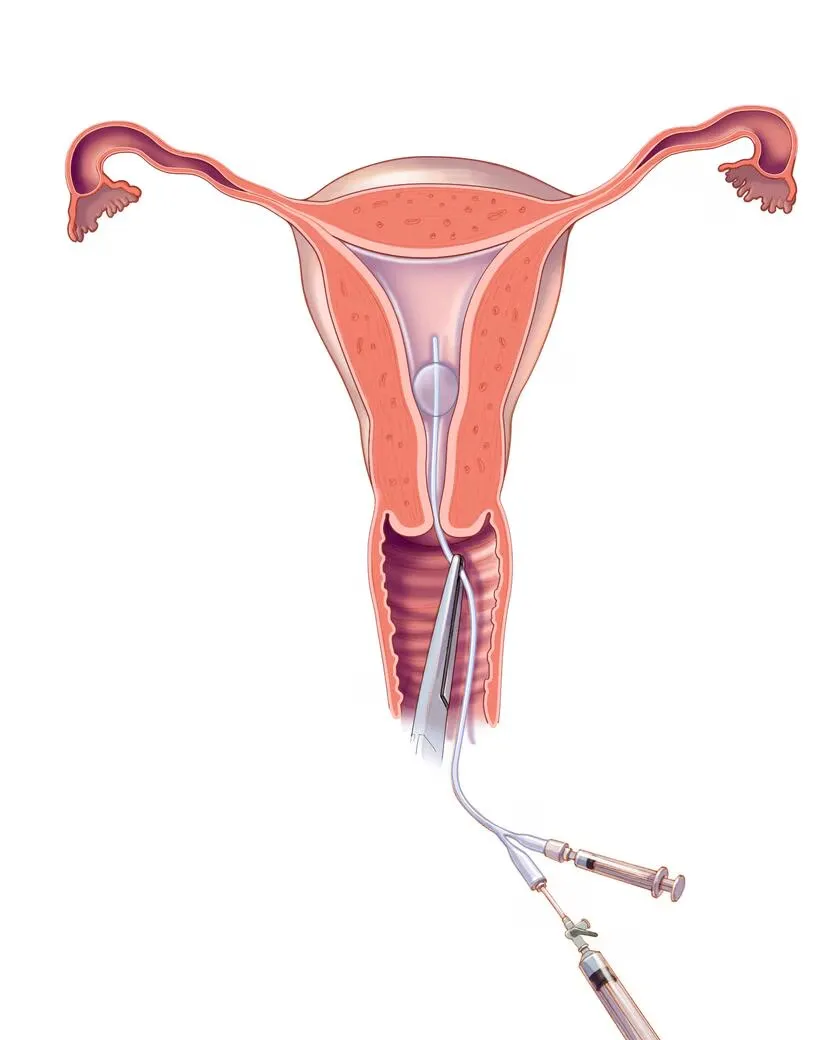
Hysterosalpingography
During this X-ray test, a contrast dye is injected into the uterus to visualize its shape and to check if the fallopian tubes are open. If any abnormalities are found, further evaluation may be recommended.
Ovarian reserve testing
This series of blood and imaging tests assesses the quality and quantity of eggs available for ovulation. It’s often recommended for women over age 35 or those at risk of reduced egg supply.
Hormone testing
Additional hormone tests evaluate thyroid, pituitary, and ovulatory hormone levels that regulate reproductive function.
Imaging tests
A pelvic ultrasound is used to identify uterine or fallopian tube abnormalities. In some cases, a sonohysterogram (saline infusion sonogram) or hysteroscopy provides detailed images of the uterine cavity that aren’t visible on standard ultrasound.
Hysterosalpingography procedure
A doctor or technician inserts a thin catheter through the cervix and releases contrast dye into the uterus. The dye outlines the uterine cavity and fallopian tubes, which become visible on X-ray.
Additional Testing (if needed)
Laparoscopy
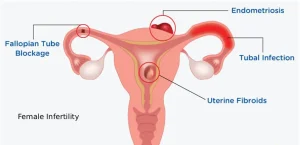
This minimally invasive surgery involves inserting a small camera through an incision near the navel to examine the uterus, fallopian tubes, and ovaries. It can detect endometriosis, scarring, blockages, or structural issues.
Genetic testing
In some cases, genetic tests are recommended to detect chromosomal or gene changes that may contribute to infertility.
Treatment
Treatment for infertility depends on the cause, age, duration of infertility, and personal preferences. Because infertility can be complex, treatment may require medical, surgical, or assisted reproductive approaches, often involving emotional, physical, and financial commitment.
Medications to Restore Fertility
Fertility drugs regulate or stimulate ovulation and are the most common treatment for women with ovulation disorders. They mimic natural hormones such as FSH (follicle-stimulating hormone) and LH (luteinizing hormone) to trigger or enhance ovulation.
Common fertility medications include:
-
Clomiphene citrate:
An oral medication that stimulates the release of FSH and LH, promoting ovulation. It’s often the first-line treatment for women under 39 who do not have PCOS. -
Gonadotropins:
Injectable hormones, including human menopausal gonadotropin (hMG) or FSH (e.g., Gonal-F, Follistim AQ, Bravelle), stimulate the ovaries to produce multiple eggs. Human chorionic gonadotropin (hCG) is used to mature and release eggs during ovulation. These medications carry a higher risk of multiple pregnancies. -
Metformin:
Used when insulin resistance contributes to infertility, especially in women with PCOS. It improves insulin sensitivity and may promote regular ovulation. -
Letrozole (Femara):
An aromatase inhibitor that works similarly to clomiphene. It’s often prescribed for women under 39 with PCOS. -
Bromocriptine (Parlodel, Cycloset):
A dopamine agonist that treats ovulation problems caused by excess prolactin production (hyperprolactinemia).
Risks of Fertility Drugs
-
Pregnancy with multiples:
Oral medications have a <10% chance of twins, while injectable medications may increase the risk up to 30% and can lead to triplets or more. Adjusting medication doses can help minimize this risk. -
Ovarian hyperstimulation syndrome (OHSS):
A rare condition that causes swollen, painful ovaries, bloating, nausea, or abdominal discomfort. Severe forms may cause rapid weight gain, fluid buildup, and breathing difficulty. -
Possible ovarian tumor risk:
Long-term use of fertility drugs (over 12 months without pregnancy) may slightly increase the risk of borderline ovarian tumors. However, this may relate more to infertility itself than to the medications.
Surgical Treatments
Surgery is less common today due to the success of other treatments but may be used to correct structural problems affecting fertility.
-
Laparoscopic or hysteroscopic surgery:
Used to treat uterine abnormalities, remove polyps or fibroids that distort the uterine cavity, or remove pelvic adhesions. -
Tubal surgery:
If fallopian tubes are blocked or damaged, laparoscopic surgery can remove adhesions or reopen the tubes. In some cases, removing or blocking severely damaged tubes can improve success rates with in vitro fertilization (IVF).
Reproductive Assistance
Intrauterine insemination (IUI):
Healthy sperm are placed directly into the uterus around ovulation to improve the chances of fertilization.
Assisted reproductive technology (ART):
The most common ART is in vitro fertilization (IVF) — where mature eggs are retrieved, fertilized with sperm in a lab, and transferred into the uterus. IVF cycles typically take several weeks and involve hormonal injections and monitoring.
Advertisement