Overview
Diagnosis
A healthcare provider begins diagnosis of fibromuscular dysplasia by performing a physical examination and asking questions about your family and medical history. Using a stethoscope, the provider listens to the arteries in the neck and abdomen to detect irregular blood flow sounds that may indicate narrowed arteries.
If a close family member has or had fibromuscular dysplasia, testing may be recommended even if you do not have symptoms.
Tests
Several tests can help confirm fibromuscular dysplasia and determine which arteries are affected.
-
Blood tests are used to check for conditions that may cause artery narrowing. These include tests for blood sugar and cholesterol levels.
-
Duplex ultrasound uses sound waves to create images of blood flow and the structure of blood vessels. A small device is pressed gently against the skin to capture these images.
-
Angiogram is a common test for fibromuscular dysplasia. A catheter is inserted into an artery and dye is injected so X-rays can clearly show the shape and condition of the arteries.
-
CT angiogram provides detailed cross-sectional images using a CT scanner. A contrast dye is injected into a vein to make blood vessels visible. This test can identify artery narrowing, aneurysms, or dissections.
-
Magnetic resonance angiogram uses magnetic fields and radio waves to produce detailed images. A contrast dye may be injected to help highlight the arteries and identify aneurysms or tears.
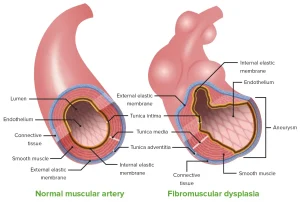
The most common appearance of fibromuscular dysplasia on imaging is described as a “string of beads,” though some cases may appear smooth.
Treatment
Treatment for fibromuscular dysplasia depends on which arteries are affected, the severity of symptoms, and other health conditions such as high blood pressure. Some people require only regular monitoring, while others may need medication or procedures to improve blood flow.
If symptoms change or an aneurysm develops, repeat imaging tests may be recommended to monitor the arteries.
Medications
When fibromuscular dysplasia causes high blood pressure, medications are often prescribed to control it.
Common types include:
-
Angiotensin-converting enzyme (ACE) inhibitors such as benazepril, enalapril, or lisinopril, which relax blood vessels.
-
Angiotensin 2 receptor blockers such as candesartan, irbesartan, losartan, or valsartan, which also help blood vessels relax.
-
Diuretics, or water pills, such as hydrochlorothiazide, used to reduce excess fluid and support other blood pressure medications.
-
Calcium channel blockers such as amlodipine or nifedipine, which relax and widen blood vessels.
-
Beta blockers such as metoprolol or atenolol, which slow the heart rate and lower blood pressure.
Because some of these medications can affect kidney function, regular blood and urine tests may be required.
A daily low-dose aspirin may sometimes be recommended to lower the risk of stroke. However, this should only be started under medical advice.
Surgery and Procedures
When arteries are severely narrowed or damaged, procedures may be needed to restore healthy blood flow.
-
Percutaneous transluminal angioplasty (PTA) uses a thin catheter with a small balloon to widen the narrowed artery. In some cases, a metal stent is placed to help keep the artery open.
-
Surgical repair or replacement of the damaged artery, known as surgical revascularization, may be considered when angioplasty is not suitable. The surgical approach depends on the artery involved and the extent of damage.
Advertisement