Overview
Diagnosis
Frontal lobe epilepsy can be challenging to diagnose because its symptoms may resemble mental health disorders or sleep disturbances such as night terrors. In some cases, seizures that appear to start in the frontal lobe may actually originate elsewhere in the brain.
To make a diagnosis, a healthcare professional reviews your medical history, discusses your symptoms, and performs a physical examination. Blood tests may be ordered to rule out other health conditions or disorders that could be causing the seizures.
You may also need a neurological examination to assess your:
-
Muscle strength
-
Sensory skills
-
Hearing and speech
-
Vision
-
Coordination and balance
Additional tests may include:
-
Brain scans: Magnetic resonance imaging (MRI) is the most common imaging test used to detect structural abnormalities or lesions in the brain. MRI produces detailed images of brain tissues using radio waves and a strong magnetic field. The test is painless but may cause discomfort for people who feel uneasy in enclosed spaces.
-
Electroencephalogram (EEG): This test records electrical activity in the brain using small electrodes placed on the scalp. EEGs can identify abnormal brain wave patterns associated with epilepsy, though they may not always detect frontal lobe seizures.
-
Video EEG monitoring: This test combines continuous EEG recording with video monitoring, usually performed overnight in a sleep clinic. It helps healthcare professionals correlate physical seizure activity with electrical changes in the brain, improving diagnostic accuracy.
Treatment
Treatment for frontal lobe epilepsy focuses on controlling seizures and improving quality of life. Over the years, new anti-seizure medications and surgical options have expanded the range of treatments available.
Medications
Anti-seizure medications are usually the first line of treatment. Most medicines are equally effective for controlling frontal lobe seizures, though not everyone becomes seizure-free. Some individuals may need to try multiple medications or a combination of drugs to achieve optimal results. Ongoing research continues to explore new and more effective medications.
Surgery
Surgery may be considered if seizures cannot be controlled with medication. The main goal of surgery is to locate and treat the area of the brain responsible for seizure activity.
Imaging and mapping techniques used before surgery include:
-
Single-photon emission computerized tomography (SPECT) and subtraction ictal SPECT coregistered to MRI (SISCOM) to pinpoint seizure origins
-
Brain mapping using implanted electrodes to identify critical brain areas
-
Functional MRI (fMRI) to map language and motor regions before surgery
Common surgical options include:
-
Removing the focal point: If seizures start in a specific brain area, removing that tissue may reduce or stop seizures.
-
Isolating the focal point: When the affected area cannot be removed, surgeons may make small cuts to prevent seizure activity from spreading.
-
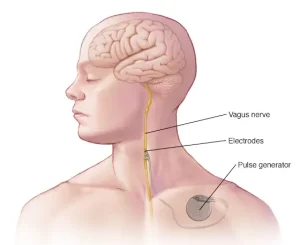
Vagus nerve stimulation: A small implanted device sends electrical impulses to the vagus nerve, helping reduce seizure frequency.
-
Responsive neurostimulation: A device implanted in the brain detects seizure activity and delivers electrical stimulation to stop it.
-
Deep brain stimulation (DBS): Electrodes implanted in the brain are connected to a generator in the chest. The device sends regular electrical impulses to disrupt abnormal brain activity.
Even after surgery, anti-seizure medications may still be required, though often at lower doses. With appropriate diagnosis and treatment, many people with frontal lobe epilepsy experience improved seizure control and a better quality of life.
Advertisement