Overview
Diagnosis
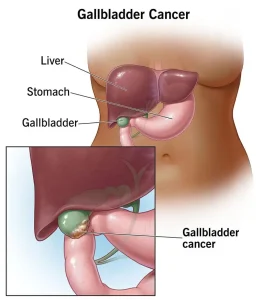
Diagnosing gallbladder cancer usually begins with a discussion about your symptoms and a physical examination. Healthcare professionals often use a combination of blood tests and imaging tests to identify signs of cancer in the gallbladder and to assess overall organ function.
Blood tests
Blood tests help evaluate how well your liver is working. Abnormal results can indicate liver or bile duct issues, which may suggest gallbladder problems or cancer.
Imaging tests
Imaging studies are essential to create detailed pictures of the gallbladder and surrounding structures. Common imaging methods include:
-
Ultrasound
-
CT scan
-
MRI
These tests help detect tumors, blockages, or other abnormalities that could indicate gallbladder cancer.
Finding the extent of gallbladder cancer
After confirming a diagnosis, the next step is determining how far the cancer has spread, a process called staging. Staging helps guide treatment decisions and provides insight into prognosis.
Tests and procedures used for staging include:
-
Tests to look at the bile ducts: Procedures such as magnetic resonance cholangiography (MRC) or endoscopic retrograde cholangiopancreatography (ERCP) use dye and imaging to check for bile duct blockages.
-
Other imaging scans: Additional CT or MRI scans of the abdomen and chest help determine whether the cancer has spread to nearby organs or distant areas.
-
Exploratory surgery: In some cases, a surgeon may perform laparoscopy, using a small incision and a camera to look inside the abdomen and check if the cancer has spread.
Based on these results, doctors assign a stage to the cancer, from stage 0 to stage 4:
-
Stage 1: Cancer is only within the gallbladder.
-
Stage 4: Cancer has grown through the gallbladder wall and may have spread to nearby organs or distant parts of the body.
Lower stages often have a better chance of successful treatment and recovery.
Treatment
Treatment options for gallbladder cancer depend on several factors, including the cancer’s stage, whether it has spread, your overall health, and personal preferences. Surgery is the most common treatment when the cancer is confined to the gallbladder. In advanced cases, non-surgical treatments may be used.
Surgery
Surgery is the main treatment for early-stage gallbladder cancer that has not spread to surrounding tissues. Common surgical options include:
-
Cholecystectomy: Removal of the gallbladder when cancer is limited to the organ itself.
-
Extended surgery: Removal of the gallbladder along with parts of the liver and bile ducts if the cancer has spread slightly beyond the gallbladder.
If the tumor is small and completely removed, additional treatments may not be necessary.
Chemotherapy
Chemotherapy uses powerful medicines to destroy cancer cells. Most chemotherapy drugs are given intravenously, though some are available in pill form. It may be used:
-
After surgery, to kill any remaining cancer cells
-
Before surgery, to shrink the tumor
-
As a primary treatment when surgery is not an option
Radiation therapy
Radiation therapy targets cancer cells with high-energy beams such as X-rays or protons. It can be used:
-
Alongside chemotherapy after surgery if all cancer cells could not be removed
-
To manage pain, jaundice, or other symptoms in advanced cases where surgery is not possible
Targeted therapy
Targeted therapy focuses on specific genetic or molecular changes in cancer cells. These medicines block certain cell functions that help cancer grow. Before starting targeted therapy, lab tests are done to determine if your cancer has the necessary genetic changes for this treatment to work effectively.
Immunotherapy
Immunotherapy strengthens the body’s immune system to detect and destroy cancer cells. Gallbladder cancer cells often evade the immune response, and immunotherapy helps the body recognize and attack them. This approach is usually used in advanced or metastatic gallbladder cancer cases.
Advertisement