Overview
Diagnosis
To determine the cause of gastrointestinal bleeding, a healthcare professional will start by reviewing your medical history and performing a physical exam. This includes discussing any previous bleeding episodes and current symptoms. Several diagnostic tests may be ordered to locate the source of the bleed.
Common tests for diagnosing GI bleeding include:
-
Blood tests
These may include a complete blood count to check for anemia, tests to measure how quickly your blood clots, platelet counts, and liver function tests. -
Stool tests
Laboratory analysis of stool samples can help identify hidden, or occult, blood and pinpoint possible sources of bleeding in the digestive tract. -
Nasogastric lavage
A tube is passed through the nose into the stomach to remove stomach contents. Examining the contents can help determine whether bleeding originates in the upper digestive tract. -
Upper endoscopy
This procedure uses a thin, flexible tube with a camera, called an endoscope, to view the upper digestive system, including the esophagus, stomach, and upper small intestine. -
Colonoscopy
A long, flexible tube with a video camera is inserted into the rectum to examine the entire large intestine and rectum. It can also be used to treat sources of bleeding such as polyps. -
Capsule endoscopy
In this noninvasive procedure, you swallow a small capsule that contains a miniature camera. As it travels through your digestive tract, it takes thousands of images that are transmitted to a recorder worn around your waist. -
Flexible sigmoidoscopy
A lighted tube with a camera is inserted into the rectum to view the rectum and the lower part of the large intestine, known as the sigmoid colon. -
Balloon-assisted enteroscopy
This specialized endoscopic test allows doctors to view areas of the small intestine that are difficult to reach with other scopes. In some cases, treatment can be performed during the same procedure. -
Angiography
A contrast dye is injected into the arteries, followed by X-rays to identify and possibly treat bleeding blood vessels or other abnormalities. -
Imaging tests
Other imaging options, such as CT scans of the abdomen, may be used to locate the source of bleeding when endoscopy or colonoscopy results are inconclusive.
If the bleeding is severe and cannot be located with noninvasive methods, surgery may be necessary to allow direct visualization of the small intestine. However, this is rarely required.
Treatment
Gastrointestinal bleeding often resolves on its own, but when it doesn’t, treatment depends on the cause and location of the bleed. Many cases can be treated with medications or procedures performed during diagnostic tests.
Treatment options for GI bleeding include:
-
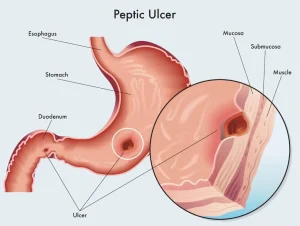
Endoscopic treatment
Bleeding peptic ulcers can often be treated during an upper endoscopy by applying clips, cauterizing tissue, or injecting medications directly at the bleeding site. Similarly, colonoscopy can be used to remove bleeding polyps or cauterize bleeding vessels. -
Medication
For upper GI bleeding, an intravenous proton pump inhibitor (PPI) may be administered to reduce stomach acid and stabilize the bleeding site. Once the cause is identified, your healthcare provider will decide whether continued PPI therapy is needed. -
Fluids and blood transfusions
In cases of significant blood loss, intravenous fluids and possibly blood transfusions may be required to restore volume and maintain stability. -
Stopping certain medications
If you are taking blood-thinning medications such as aspirin, anticoagulants, or nonsteroidal anti-inflammatory drugs (NSAIDs), your healthcare provider may advise stopping them temporarily to prevent further bleeding.
Most patients recover fully once the bleeding source is identified and treated. However, ongoing monitoring is important to prevent recurrence and manage any underlying conditions contributing to the bleed.
Advertisement