Overview
Diagnosis
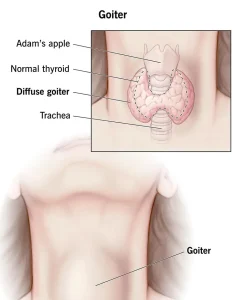
A goiter is often discovered during a routine physical exam. By feeling your neck, a healthcare provider may detect an enlarged thyroid, a single nodule, or multiple nodules. Occasionally, a goiter is found during imaging tests for unrelated conditions.
Additional tests help to:
-
Measure the size of the thyroid
-
Detect any nodules
-
Assess whether the thyroid is overactive or underactive
-
Determine the underlying cause of the goiter
Common tests include:
-
Thyroid function tests: Blood tests measure Thyroid-stimulating Hormone (TSH), Thyroxine (T-4), and Triiodothyronine (T-3) to check thyroid activity.
-
Antibody test: Detects antibodies linked to autoimmune disorders such as Hashimoto’s disease or Graves’ disease.
-
Ultrasonography: Uses sound waves to create images of the thyroid, showing its size and any nodules.
-
Radioactive iodine uptake: Measures how much and how quickly the thyroid absorbs iodine, helping assess function and cause.
-
Biopsy: Fine-needle aspiration guided by ultrasound collects tissue or fluid from nodules to check for cancerous cells.
Treatment
Treatment depends on the size of the goiter, symptoms, and the underlying cause. Small goiters with normal thyroid function may simply be monitored with regular checkups.
Medications may include:
-
Increasing hormone production: Thyroid hormone replacements such as levothyroxine (T-4) or liothyronine (T-3) for underactive thyroid can also reduce goiter size.
-
Reducing hormone production: Anti-thyroid drugs like methimazole (Tapazole) help manage an overactive thyroid and may shrink the goiter.
-
Blocking hormone activity: Beta blockers, including atenolol and metoprolol, can reduce symptoms of hyperthyroidism.
-
Managing pain: Pain or inflammation may be treated with NSAIDs such as aspirin, ibuprofen, or naproxen sodium; severe cases may require corticosteroids.
Surgery may be needed for goiters that cause:
-
Difficulty breathing or swallowing
-
Hyperthyroidism from thyroid nodules
-
Thyroid cancer
Surgery can be a total or partial thyroidectomy. Thyroid hormone replacement may be required depending on the amount removed.
Radioactive iodine treatment can reduce the size of an overactive thyroid by destroying thyroid cells. Hormone replacement therapy may also be needed after treatment to maintain normal hormone levels.
Early detection and proper management help prevent complications and maintain healthy thyroid function.
Advertisement