Overview
Diagnosis
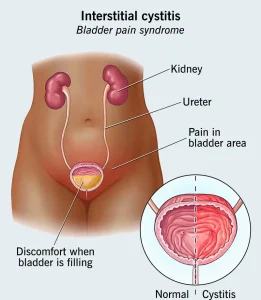
Diagnosis of interstitial cystitis involves several steps to understand symptoms, rule out infections and assess bladder health. Your health care provider may begin with a detailed medical history and ask you to maintain a bladder diary to track fluid intake and urine output.
A pelvic exam may be done to evaluate the external genitals, vagina, cervix and internal pelvic organs. A urine test is often performed to check for signs of infection.
Cystoscopy allows your provider to view the bladder lining using a thin tube with a camera. During this procedure, the bladder may be filled with liquid to measure capacity, a process known as hydrodistention. In some cases, a biopsy of the bladder or urethra may be taken to rule out cancer or other rare causes of bladder pain.
Additional tests may include urine cytology to examine bladder cells or a potassium sensitivity test, which helps identify bladder lining sensitivity. A noticeable increase in pain or urgency when potassium solution is placed in the bladder may support the diagnosis of interstitial cystitis.
Treatment
Treatment for interstitial cystitis varies widely because symptoms differ from person to person. Many people need to try multiple options or a combination of therapies before finding meaningful relief.
Physical therapy can be especially helpful for those with pelvic pain linked to muscle tenderness or pelvic floor dysfunction. Techniques focus on relaxing tight muscles and improving connective tissue mobility.
Oral medications may also play a role. These include anti-inflammatory drugs for pain relief, tricyclic antidepressants to relax the bladder and decrease pain, and antihistamines to reduce urgency and frequency. Pentosan polysulfate sodium may help protect the bladder lining, though results often take several months. Regular eye exams may be needed due to possible effects on the retina.
Nerve stimulation techniques, such as transcutaneous electrical nerve stimulation, use mild electrical pulses to reduce pelvic pain and urinary frequency. Sacral nerve stimulation targets nerves connected to bladder function and may help control urgency when other treatments have not worked.
Bladder distention done during cystoscopy may temporarily improve symptoms for some people. In certain cases, botulinum toxin A may be injected into the bladder wall, though it may cause difficulty emptying the bladder.
Bladder instillation involves placing medications such as dimethyl sulfoxide into the bladder through a catheter. Treatment schedules vary, with initial weekly sessions often followed by maintenance treatments.
Surgery is rarely used and is reserved for severe cases when other therapies have failed. Procedures may include removing ulcers through fulguration or resection, or bladder augmentation to increase bladder capacity. Surgery does not always relieve pain, and some people may need to use a catheter regularly after the procedure.
Advertisement