Overview
Diagnosis
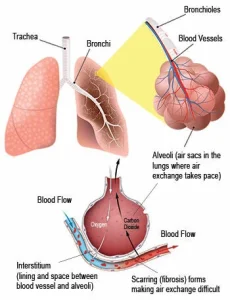
Diagnosis of interstitial lung disease can be difficult because many conditions share similar symptoms. In some cases, the exact cause cannot be identified. Healthcare professionals must rule out other diseases before confirming ILD. Various tests are used to understand lung function, identify inflammation and assess the extent of lung damage.
Lab tests may include bloodwork to detect proteins, antibodies or markers linked to autoimmune conditions or environmental exposures such as mold or bird protein.
Imaging tests often begin with a CT scan, which is central to diagnosing ILD. High-resolution CT scans show detailed images of lung scarring and help determine how advanced the disease is. An echocardiogram may also be used to check how the heart is functioning and measure pressure in the right side of the heart.
Pulmonary function tests such as spirometry measure how much air your lungs can hold, how quickly you can exhale and how well oxygen passes from your lungs into your bloodstream. Oximetry may be used to check oxygen levels at rest or during activity.
Lung tissue analysis is sometimes required for an accurate diagnosis. A bronchoscopy may be performed to collect small tissue samples. Bronchoalveolar lavage gathers cells from the air sacs using a saline solution. In some cases, a surgical biopsy performed under general anesthesia is needed to obtain a sample large enough for diagnosis.
Treatment
Treatment for interstitial lung disease focuses on slowing the progression of damage, managing symptoms and improving quality of life. Existing lung scarring cannot be reversed, but certain therapies may help relieve symptoms or slow the disease.
Medications are often used based on the specific type and cause of ILD. Corticosteroids such as prednisone may be given first to reduce inflammation. Some people may require additional immune-suppressing drugs. Medicines like pirfenidone and nintedanib can slow the progression of idiopathic pulmonary fibrosis and may also help slow fibrosis from other ILD types. If you have symptoms of acid reflux, your care plan may include treatments to reduce stomach acid.
Oxygen therapy may be recommended to support breathing, improve exercise tolerance, reduce complications caused by low oxygen levels and enhance sleep and overall well-being. Some people need oxygen only during sleep or activity, while others may require it throughout the day.
Pulmonary rehabilitation programs help improve daily functioning. These programs include education about lung disease, exercise training, breathing techniques, emotional support and nutritional counseling.
In severe cases when other treatments are not effective, a lung transplant may be considered as a last-resort option.
Advertisement