Overview
Diagnosis
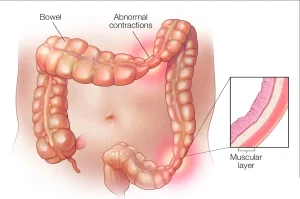
Diagnosing irritable bowel syndrome (IBS) involves reviewing medical history, completing a physical exam and ruling out other conditions such as celiac disease or inflammatory bowel disease. Once other causes are excluded, healthcare professionals may use diagnostic guidelines such as the Rome criteria, which look for weekly belly pain over the last three months along with changes in stool frequency, consistency or relief after passing stool.
IBS also is categorized into types to guide treatment. These include constipation-predominant, diarrhea-predominant, mixed and unclassified.
Healthcare professionals also check for warning signs that may suggest conditions other than IBS. These signs can include symptoms beginning after age 50, weight loss, rectal bleeding, fever, nausea, nighttime abdominal pain, ongoing diarrhea, vomiting or anemia related to low iron. If these symptoms are present or treatment does not work, more evaluation is needed.
Additional tests
To help with diagnosis, several tests and procedures may be recommended.
Tests may include:
-
Colonoscopy to view the entire colon
-
CT scan to look at the abdomen and pelvis
-
Upper endoscopy when symptoms suggest an upper digestive disorder or celiac disease
-
Lactose intolerance tests using breath testing or dietary trials
-
Breath tests for bacterial overgrowth
-
Stool studies to look for infection, parasites, malabsorption or bile acid issues
Treatment
Treatment for IBS focuses on relieving symptoms and improving quality of life. Mild symptoms can often be managed with lifestyle changes, stress management and dietary adjustments.
Dietary and lifestyle changes
A healthcare professional may recommend:
-
Avoiding trigger foods
-
Eating high-fiber foods
-
Drinking enough fluids
-
Exercising regularly
-
Getting adequate sleep
Some foods may need to be limited or removed, depending on symptoms. These include:
-
High-gas foods, such as carbonated drinks
-
Gluten-containing foods, which may worsen diarrhea for some
-
FODMAP-containing foods, which include certain fruits, vegetables, grains and dairy products
Dietitians can help guide these changes, especially when following a low-FODMAP diet.
Counseling
For moderate to severe symptoms, counseling or therapy may be recommended, especially if stress or depression worsens symptoms.
Medicines based on symptoms
Several medicines may help depending on the type of IBS and key symptoms.
Options include:
-
Fiber supplements such as psyllium to help with constipation
-
Laxatives if fiber does not improve constipation
-
Antidiarrheal medicines, including loperamide or bile acid binders
-
Anticholinergic medicines for bowel spasms
-
Tricyclic antidepressants to help reduce pain
-
SSRI antidepressants for people with depression and constipation-related IBS
-
Pain medicines such as pregabalin or gabapentin for severe pain or bloating
Medicines specifically for IBS
Certain prescription medicines may be used for specific types of IBS.
These include:
-
Alosetron for severe diarrhea-predominant IBS in women who have not responded to other treatments
-
Eluxadoline to reduce bowel contractions and ease diarrhea
-
Rifaximin to address bacterial overgrowth and diarrhea
-
Lubiprostone for women with constipation-predominant IBS
-
Linaclotide to improve constipation by increasing fluid in the intestines
Potential future treatments
Researchers are studying fecal microbiota transplantation (FMT) as a possible treatment. This procedure aims to restore healthy intestinal bacteria. It is still considered investigational, and clinical trials are ongoing.
Advertisement