Overview
Diagnosis
Diagnosis of Perthes disease begins with a physical exam. During the exam, a healthcare professional gently moves your child’s legs into different positions to assess range of motion and identify movements that cause pain.
Imaging tests play a key role in confirming the condition and may include:
-
X-rays, which may appear normal at first. Changes linked to Perthes disease often become visible 1 to 2 months after symptoms begin. Multiple X-rays over time help track disease progression.
-
MRI, which uses magnetic fields and radio waves to create detailed images. It can often show bone damage more clearly than X-rays, but it is not always required.
Treatment
Treatment for Perthes disease can take several years. The recommended approach depends on the child’s age at symptom onset, the stage of the disease, and the degree of hip damage.
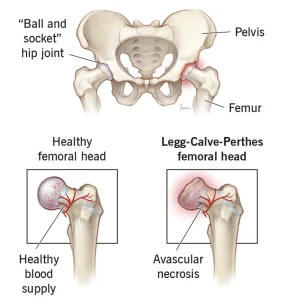
As the condition progresses, the femoral head weakens and can break apart. During healing, the hip socket can act like a mold that helps the femoral head stay round. For this to work well, the femoral head must fit securely within the socket.
Some children may need a special leg cast that keeps the legs spread apart for 4 to 6 weeks to maintain proper positioning. Others may require surgery to ensure the femoral head stays aligned within the socket. Surgical procedures often involve making wedge-shaped cuts in the thighbone or pelvis to restore alignment. Surgery is usually not needed for children under 6 because their hip joints naturally reshape more easily.
Other treatments
Many younger children or those with mild disease may only need observation or conservative care. Options may include:
-
Activity restrictions to prevent worsening hip damage by avoiding running, jumping or other high-impact movements.
-
Crutches to limit weight-bearing on the affected hip.
-
Physical therapy to maintain flexibility through stretching exercises as the hip becomes stiff.
-
Anti-inflammatory medicines such as ibuprofen to help relieve pain.
Advertisement