Overview
Diagnosis
Your healthcare provider will review your medical history and perform a physical exam, including a pelvic exam. During the pelvic exam, your provider checks for anything unusual with the reproductive organs and looks for signs of infection.
Additional tests may include:
-
Ultrasound. Uses sound waves to create images of the uterus, cervix, fallopian tubes, and ovaries.
-
Other imaging tests. CT or MRI scans provide more detailed images than an ultrasound. CT combines X-rays from multiple angles to produce cross-sectional images of bones, organs, and soft tissues. MRI uses radio waves and a strong magnetic field to produce detailed images of internal structures. Both tests are noninvasive and painless.
-
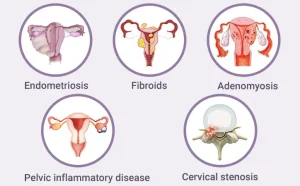
Laparoscopy. While not usually necessary, laparoscopy can detect underlying conditions like endometriosis, adhesions, fibroids, ovarian cysts, or ectopic pregnancy. During this outpatient procedure, tiny incisions are made in the abdomen, and a fiber-optic tube with a camera allows the doctor to view the abdominal cavity and reproductive organs.
Treatment
To relieve menstrual cramps, your healthcare provider may recommend:
-
Pain relievers. Over-the-counter medicines such as ibuprofen or naproxen sodium can help control cramp pain. Prescription NSAIDs are also available. Start taking the medicine at the beginning of your period or when symptoms start and continue as directed for two to three days or until symptoms subside.
-
Hormonal birth control. Pills, injections, skin patches, implants, vaginal rings, or intrauterine devices (IUDs) containing hormones prevent ovulation and reduce the severity of cramps.
-
Surgery. If cramps are caused by conditions like endometriosis or fibroids, surgery may relieve symptoms. In some cases, removal of the uterus may be considered if other treatments fail and if you do not plan to have children.
Advertisement