Overview
Diagnosis
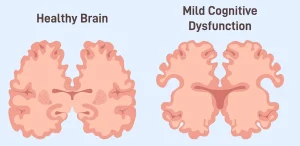
There is no single test that can diagnose mild cognitive impairment, also known as MCI. A diagnosis is based on the information you provide, a detailed medical evaluation and the results of specific tests. Healthcare professionals often use diagnostic criteria developed by international experts.
Key features used to diagnose MCI include:
-
Changes in memory or other mental abilities
Symptoms may involve problems with memory, planning, following instructions or making decisions. These changes are often confirmed by a family member or close friend. -
Mental ability that declines over time
A careful medical history shows gradual change, supported by observations from someone who knows you well. -
Daily activities are not significantly affected
Although symptoms may be concerning, people with MCI are generally able to manage daily life independently. -
Mild changes on mental status testing
Brief tests such as the Short Test of Mental Status, Montreal Cognitive Assessment or Mini-Mental State Examination may show changes beyond what is expected for age and education. More detailed testing helps define which mental abilities are affected. -
The diagnosis is not dementia
Symptoms are not severe enough to meet criteria for Alzheimer’s disease or another form of dementia.
Neurological exam
As part of the physical examination, a healthcare professional may assess how well the brain and nervous system are functioning. This helps identify conditions that may affect memory and thinking.
The neurological exam may include testing of:
-
Reflexes
-
Eye movements
-
Walking and balance
If MCI is suspected to be related to early Alzheimer’s disease, tests may be done to detect biomarkers. These involve identifying protein buildup in the brain through blood tests, spinal fluid tests or specialized brain scans. The presence of these biomarkers suggests that MCI symptoms may be due to mild Alzheimer’s disease.
Lab tests
Blood tests can help rule out physical causes of memory problems, such as vitamin B-12 deficiency or thyroid disorders. Some blood and spinal fluid tests also check for proteins associated with Alzheimer’s disease and may help confirm the cause of cognitive impairment.
Brain imaging
Brain imaging tests such as MRI or CT scans can look for tumors, strokes or bleeding. Positron emission tomography scans may be used to detect protein buildup linked to Alzheimer’s disease.
Mental status testing
Short mental status tests usually take about 10 minutes and assess tasks such as recalling the date and following instructions. Longer tests compare mental abilities with others of similar age and education and can reveal patterns that help identify the cause of symptoms.
Treatment
Treatment for mild cognitive impairment depends on the underlying cause. If symptoms are related to medicines or other health conditions, treatment focuses on correcting those issues. Research into MCI is ongoing, with clinical studies aimed at improving symptoms or delaying dementia.
Alzheimer’s disease medicines
For people with MCI due to Alzheimer’s disease, healthcare professionals may recommend medicines approved by the FDA to slow decline in thinking and memory. These medicines help reduce the buildup of amyloid plaques in the brain and require a brain MRI before starting treatment.
Approved medicines include:
-
Lecanemab-irmb
Given as an IV infusion every two weeks, with possible side effects such as flu-like symptoms, nausea, dizziness and breathing difficulties. -
Donanemab-azbt
Given as an IV infusion every four weeks, with side effects that may include headache, nausea, flu-like symptoms and changes in blood pressure.
These medicines can also cause brain swelling or small brain bleeds. Certain genetic factors, such as having the APOE e4 gene, increase the risk of serious side effects. Regular brain MRIs are needed during treatment. Blood thinners can further increase bleeding risk and should be discussed with a healthcare professional.
Cholinesterase inhibitors may sometimes be prescribed when memory loss is the main symptom, but they are not recommended for routine treatment of MCI and have not been proven to prevent dementia.
Treating reversible causes of MCI: stopping certain medicines
Some medicines can cause thinking and memory problems that improve once the medicine is stopped. Always discuss this with your healthcare professional before making changes. Medicines that may contribute include:
-
Benzodiazepines
-
Anticholinergic medicines
-
Antihistamines
-
Opioids
-
Proton pump inhibitors
Treating reversible causes of MCI: addressing other conditions
Other medical conditions can worsen memory and thinking. Treating these conditions may improve cognitive symptoms.
Common examples include:
-
High blood pressure, which can affect blood vessels in the brain
-
Depression, which can cause mental fog and forgetfulness
-
Sleep apnea, which disrupts sleep and affects attention and memory
Managing these conditions can help support brain health and improve overall quality of life for people with mild cognitive impairment.
Advertisement