Overview
Diagnosis
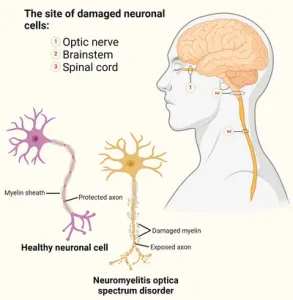
Diagnosing neuromyelitis optica (NMO) involves a physical exam, medical history review, and tests to rule out other conditions with similar symptoms. The International Panel for NMO Diagnosis established criteria in 2015 for neuromyelitis optica spectrum disorder (NMOSD).
-
Neurological exam: A neurologist evaluates movement, muscle strength, coordination, sensation, memory, thinking, vision, and speech. An eye doctor may also be involved.
-
MRI: Imaging of the brain, optic nerves, and spinal cord can show lesions or damaged areas.
-
Blood tests: Tests may detect aquaporin-4 immunoglobulin G (AQP4-IgG), an autoantibody linked to NMO. Other biomarkers like GFAP and neurofilament light chain may help detect relapses. MOG-IgG antibody testing may rule out similar inflammatory disorders.
-
Lumbar puncture: A spinal tap checks spinal fluid for immune cells, proteins, and antibodies to distinguish NMO from MS. White blood cell levels may be higher during NMO attacks.
-
Evoked potentials test: Electrodes measure the brain’s response to visual, auditory, or sensory stimuli to detect lesions in nerves, optic nerves, spinal cord, or brainstem.
-
Optical coherence tomography: This test measures retinal nerve fiber thickness and can show vision loss caused by NMO.
Treatment
There is no cure for neuromyelitis optica, but treatments aim to reverse symptoms and prevent future attacks.
-
Reversing recent symptoms:
-
Corticosteroids such as methylprednisolone may be given intravenously for about five days, then tapered.
-
Plasma exchange may be used alone or with steroids to remove harmful substances from the blood.
-
-
Preventing future attacks:
-
Low-dose corticosteroids may reduce the risk of relapses.
-
Monoclonal antibodies, including eculizumab, satralizumab, inebilizumab, ravulizumab, and rituximab, have shown effectiveness in reducing relapses and are FDA-approved for adults.
-
Immunosuppressive medicines such as azathioprine, mycophenolate, methotrexate, cyclophosphamide, or tocilizumab may be prescribed.
-
Intravenous immunoglobulins can help decrease relapse rates.
-
Healthcare professionals may also manage associated symptoms such as pain or muscle problems to improve quality of life.
Preparing for your appointment
Before seeing your healthcare professional, prepare by:
-
Writing down symptom details, timing, and patterns.
-
Listing metal products that contact your skin.
-
Listing medications, vitamins, and supplements, including doses and reasons.
-
Preparing questions for your healthcare professional, such as the likely cause of the rash, alternative causes, expected side effects, and options for nonprescription treatments.
Your healthcare professional will likely ask about:
-
Symptom onset and location of the rash.
-
Other associated symptoms.
-
Jewelry use and occupational exposures.
-
Changes in symptoms over time.
-
Home treatments tried and their effects.
-
Factors that worsen your symptoms.
Advertisement