Overview
Diagnosis
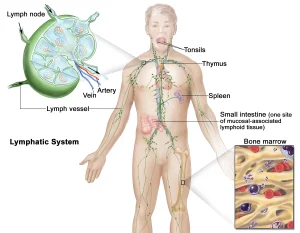
Non-Hodgkin lymphoma diagnosis often begins with a physical exam to check for swollen lymph nodes in the neck, underarms, and groin, as well as an enlarged spleen or liver. Additional tests and procedures may include blood tests, imaging tests, and tissue sampling for lab analysis.
-
Blood tests: Blood tests may detect non-Hodgkin lymphoma cells and check for viruses such as HIV, hepatitis B, and hepatitis C. Blood tests also measure lactate dehydrogenase (LDH) levels, which are often elevated in lymphoma.
-
Imaging tests: MRI, CT, and PET scans can provide images showing the location and extent of lymphoma.
-
Biopsy: A lymph node or tissue biopsy removes a sample for lab testing to identify cancer cells. The sample may come from other areas depending on symptoms and imaging results.
-
Bone marrow biopsy and aspiration: Cells are collected from the bone marrow, usually from the hip bone, to examine the presence of lymphoma. Aspiration removes liquid marrow, while a biopsy removes a small amount of solid tissue.
-
Lumbar puncture: A spinal tap collects cerebrospinal fluid to check for cancer cells, particularly if neurological symptoms are present or there is a higher risk of central nervous system involvement.
-
Laboratory analysis: Lymphoma cells from biopsy or bone marrow samples are tested for surface proteins and DNA changes. These results help determine the type of non-Hodgkin lymphoma.
Treatment
Treatment for non-Hodgkin lymphoma depends on the type, stage, growth rate, overall health, and patient preference. Options may include a watch-and-wait approach, chemotherapy, immunotherapy, targeted therapy, CAR-T cell therapy, bone marrow transplant, and radiation therapy.
-
Watch and wait: For slow-growing lymphomas without symptoms, regular checkups may be recommended to monitor cancer progression.
-
Chemotherapy: Uses strong medicines to kill cancer cells. Most are given intravenously, though some are oral. Chemotherapy may be combined with targeted therapy.
-
Immunotherapy: Medicines help the immune system recognize and destroy cancer cells. It may be combined with chemotherapy or used for refractory or relapsed lymphoma.
-
Targeted therapy: Medicines block specific chemicals in cancer cells, causing them to die. Targeted therapy can be used alone or with chemotherapy.
-
CAR-T cell therapy: White blood cells are modified in a lab to target lymphoma cells and then returned to the body to destroy the cancer. This may be used for refractory or relapsed lymphoma.
-
Bone marrow transplant: Healthy stem cells replace damaged cells after chemotherapy or radiation. Stem cells may come from the patient or a donor. This treatment is considered for relapsed or refractory lymphoma.
-
Radiation therapy: Uses powerful energy beams to target cancer. It may be the sole treatment for slow-growing lymphoma in one or two spots or used after chemotherapy to kill remaining cells and relieve symptoms.
Side effects of treatment
Treatments may cause nausea, vomiting, fatigue, fever, rash, diarrhea, infection, and more. Serious side effects can include:
-
Bone marrow suppression, increasing infection risk
-
Febrile neutropenia, a dangerous condition due to low neutrophils
-
Medicine toxicity affecting organs
-
Reactivation of viruses such as hepatitis B or C
-
Tumor lysis syndrome, a complication from rapid cancer cell breakdown
-
Infertility, depending on treatment used
Close monitoring by your healthcare team can help manage side effects and ensure the best outcome.
Advertisement