Overview
Diagnosis
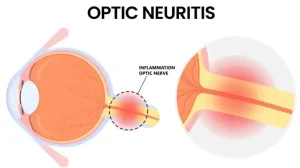
Optic neuritis is typically diagnosed by an ophthalmologist based on your medical history and a comprehensive eye examination. The goal is to determine whether inflammation of the optic nerve is present and to rule out other possible causes of vision loss.
Common diagnostic steps and tests include:
-
Routine eye exam: This includes checking vision sharpness, color perception, and side (peripheral) vision to identify any areas of vision loss.
-
Ophthalmoscopy: A bright light is used to examine the back of the eye, including the optic disk, where the optic nerve enters the retina. Swelling of the optic disk is seen in about one-third of people with optic neuritis.
-
Pupillary light reaction test: The doctor moves a light across the eyes to assess how the pupils react. In optic neuritis, the affected eye’s pupil often shows a weaker response to light.
Additional tests that may be used to confirm the diagnosis include:
-
Magnetic resonance imaging (MRI): MRI scans create detailed images of the optic nerve and brain. A contrast dye may be used to highlight inflammation. MRI can reveal lesions in the brain that may indicate a higher risk of developing multiple sclerosis (MS).
-
Blood tests: These can identify infections or specific antibodies linked to conditions such as neuromyelitis optica or MOG antibody disease.
-
Optical coherence tomography (OCT): This imaging test measures the thickness of the retinal nerve fiber layer, which may become thinner due to optic nerve damage.
-
Visual field test: Measures peripheral vision to detect areas of vision loss caused by optic neuritis.
-
Visual evoked response (VER): Electrodes attached to the head record brain activity while viewing a visual pattern. A slower response may indicate optic nerve damage.
Follow-up exams are typically scheduled two to four weeks after symptoms begin to confirm the diagnosis and monitor recovery.
Treatment
In many cases, optic neuritis improves naturally without medical intervention. However, treatments can help speed up recovery or reduce inflammation when necessary.
-
Steroid therapy: Intravenous (IV) steroids are often prescribed to reduce inflammation and accelerate vision recovery. Common side effects include weight gain, mood changes, facial flushing, stomach upset, and insomnia.
-
Plasma exchange therapy: In cases where vision loss is severe and unresponsive to steroids, plasma exchange therapy may help some individuals regain vision, although its effectiveness is still being studied.
Preventing Multiple Sclerosis (MS)
People with optic neuritis who have two or more brain lesions on MRI scans may be at a higher risk of developing MS. Preventive treatment may include:
-
Interferon beta-1a or beta-1b medications: These injectable therapies can delay or reduce the likelihood of developing MS. Possible side effects include flu-like symptoms, injection site irritation, and depression.
Prognosis
Most people recover nearly normal vision within six months after an episode of optic neuritis.
Recurrent optic neuritis may increase the risk of developing MS, neuromyelitis optica, or MOG antibody-associated disorder. When optic neuritis occurs without an underlying condition, long-term vision outcomes are generally more favorable. Regular monitoring and follow-up care with an ophthalmologist or neurologist are essential for managing and preventing recurrence.
Advertisement