Overview
Diagnosis
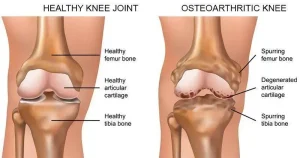
To diagnose osteoarthritis, your healthcare professional begins with a physical examination to check for tenderness, swelling, and flexibility in the affected joint. A combination of imaging and lab tests may be used to confirm the diagnosis and rule out other possible causes of joint pain.
Imaging tests
To visualize the affected joint and assess damage, the following imaging methods may be recommended:
• X-rays: While cartilage doesn’t appear on X-ray images, cartilage loss can be seen through a narrowing of the space between bones. Bone spurs may also be visible around the joint.
• Magnetic resonance imaging (MRI): MRI scans use radio waves and a strong magnetic field to create detailed images of bones and soft tissues, including cartilage. MRI is typically used in complex or unclear cases.
Lab tests
Analyzing blood or joint fluid can help support the diagnosis and rule out other conditions.
• Blood tests: While no specific blood test exists for osteoarthritis, tests can rule out conditions like rheumatoid arthritis.
• Joint fluid analysis: A sample of fluid drawn from the affected joint is tested to identify whether inflammation, infection, gout, or other conditions are causing the pain.
Treatment
Although osteoarthritis cannot be reversed, treatments can reduce pain, improve mobility, and enhance quality of life.
Medicines
Common medications used for osteoarthritis include:
• Acetaminophen: Effective for mild to moderate pain but can cause liver damage if taken in excessive doses.
• Nonsteroidal anti-inflammatory drugs (NSAIDs): Medications like ibuprofen and naproxen sodium relieve pain and inflammation. Topical NSAIDs applied as gels may provide similar relief with fewer side effects.
• Duloxetine: Originally developed as an antidepressant, duloxetine is also approved for managing chronic pain, including osteoarthritis.
Therapy
Therapeutic approaches aim to improve joint function and reduce pain.
• Physical therapy: Exercises strengthen muscles around the joint and improve flexibility. Low-impact activities such as swimming or walking can be equally effective.
• Occupational therapy: Helps modify daily activities to reduce stress on painful joints. For example, using tools with larger grips or installing a shower bench can help ease joint strain.
• Transcutaneous electrical nerve stimulation (TENS): Uses mild electrical currents to temporarily relieve pain in areas such as the knees and hips.
Surgical and other procedures
If conservative treatments fail to provide relief, surgical options may be considered.
• Cortisone injections: Corticosteroid injections can reduce inflammation and pain temporarily but are limited in frequency due to potential joint damage.
• Lubrication injections: Hyaluronic acid injections may provide cushioning in the joint, though results vary among individuals.
• Realigning bones (osteotomy): This surgical procedure reshapes bones around the knee to shift weight away from the damaged area, reducing pressure and pain.
• Joint replacement: Involves removing the damaged joint surfaces and replacing them with artificial components made of metal and plastic. Commonly performed on hips and knees, joint replacement can significantly reduce pain and restore movement.
These treatment options aim to manage pain, preserve joint function, and improve overall quality of life for people living with osteoarthritis.
Advertisement