Overview
Diagnosis
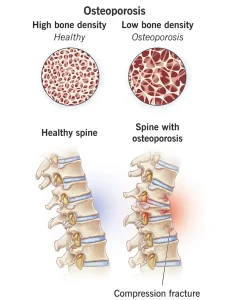
Osteoporosis is often diagnosed during routine screening or when a bone fracture is detected through X-ray imaging. In some cases, it may be discovered incidentally during imaging tests performed for other reasons, such as a chest X-ray.
During a physical exam, your healthcare professional may check for signs such as reduced height, changes in posture, or spinal curvature. To confirm the diagnosis, a bone density test is commonly performed.
A bone density test uses a low-dose X-ray machine to measure the mineral content in your bones. This painless procedure typically focuses on the hip and spine, where osteoporosis is most likely to cause fractures. During the test, you lie on a padded table while a scanner passes over your body to measure bone strength and density.
Treatment
Treatment for osteoporosis depends on the results of your bone density test and your Fracture Risk Assessment Tool (FRAX) score, which estimates your 10-year fracture risk. If your risk is low, lifestyle modifications may be recommended instead of medications. These can include improving diet, increasing physical activity, and reducing fall risks.
When medication is needed, several options are available.
Bisphosphonates
These are the most commonly prescribed drugs to prevent bone loss and fractures. Examples include:
-
Alendronate (Binosto, Fosamax)
-
Risedronate (Actonel, Atelvia)
-
Ibandronate
-
Zoledronic acid (Reclast, Zometa)
Possible side effects include nausea, abdominal discomfort, and heartburn-like symptoms. Intravenous forms may cause fever, headache, or muscle pain. Rare complications include thighbone fractures and osteonecrosis of the jaw, especially after dental surgery.
Denosumab (Prolia, Xgeva)
This medication is given as an injection every six months and offers similar or better results than bisphosphonates. It also carries the same rare risks of thighbone fractures and osteonecrosis of the jaw. Stopping denosumab suddenly may increase the risk of spinal fractures, so continuous treatment is often recommended.
Hormone-related therapy
-
Estrogen therapy can help maintain bone density after menopause but may increase the risk of breast cancer, stroke, and blood clots. It’s usually prescribed for younger women or those with menopausal symptoms.
-
Raloxifene (Evista) acts like estrogen in the bones, improving bone strength and lowering certain breast cancer risks. However, it can cause hot flashes and raise the risk of blood clots.
-
In men, testosterone replacement therapy can improve symptoms of low testosterone, but osteoporosis-specific medications are typically more effective for improving bone density.
Bone-building medicines
For severe osteoporosis or when standard treatments are ineffective, bone-stimulating drugs may be used, including:
-
Teriparatide (Bonsity, Forteo): Mimics parathyroid hormone to stimulate bone growth; given as a daily injection for up to two years.
-
Abaloparatide (Tymlos): Works similarly to Teriparatide and is also limited to two years of use.
-
Romosozumab (Evenity): A monthly injection that promotes new bone formation and is typically used for one year.
After completing bone-building therapy, it’s essential to continue with another osteoporosis medication to help maintain the newly formed bone density and prevent bone loss.
Advertisement