Overview
Diagnosis
Diagnosing ovarian cancer typically begins with a review of your symptoms, medical history, and a thorough physical examination. To confirm the diagnosis and determine the extent of the disease, your doctor may recommend a combination of tests and procedures.
Tests and procedures used to diagnose ovarian cancer include:
-
Pelvic exam: During a pelvic exam, your doctor inserts gloved fingers into your vagina and simultaneously presses a hand on your abdomen to feel your pelvic organs. The doctor also visually examines your external genitalia, vagina, and cervix.
-
Imaging tests: Ultrasound or CT scans of your abdomen and pelvis help determine the size, shape, and structure of your ovaries.
-
Blood tests: These tests may include organ function tests to assess your overall health. Your doctor might also order blood tests for tumor markers, such as the CA-125 test, which detects a protein often found on the surface of ovarian cancer cells. While these tests cannot confirm cancer alone, they can offer important diagnostic clues.
-
Surgery: In some cases, surgery to remove an ovary is necessary to confirm the diagnosis by testing the tissue for cancer cells.
-
Genetic testing: Your doctor may suggest genetic testing to identify mutations, such as BRCA1 or BRCA2, that increase ovarian cancer risk. Identifying genetic mutations can guide treatment decisions and alert family members to potential inherited risks.
Once ovarian cancer is confirmed, your doctor assigns a stage based on test results. Staging ranges from 1 to 4 (I to IV).
-
Stage 1 indicates that cancer is limited to the ovaries.
-
Stage 4 means the cancer has spread to distant parts of the body.
Treatment
Treatment for ovarian cancer typically involves a combination of surgery and chemotherapy, though other therapies may be added depending on the cancer type and stage.
Surgery
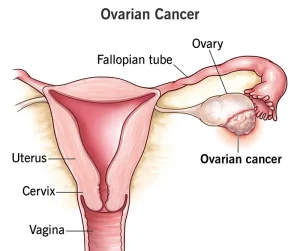
Operations to remove ovarian cancer may include:
-
Surgery to remove one ovary and its fallopian tube for early-stage cancer confined to one ovary.
-
Surgery to remove both ovaries and fallopian tubes if cancer affects both sides but hasn’t spread further.
-
Surgery to remove both ovaries, fallopian tubes, uterus, lymph nodes, and nearby fatty tissue (omentum) for more advanced cases.
-
Surgery for advanced cancer, where the goal is to remove as much of the tumor as possible, sometimes followed or preceded by chemotherapy.
Chemotherapy
Chemotherapy uses powerful drugs to kill fast-growing cancer cells. It can be administered intravenously or orally. It is often used after surgery to destroy remaining cancer cells but may also be used before surgery.
In specific cases, heated chemotherapy (hyperthermic intraperitoneal chemotherapy) is applied directly into the abdomen during surgery to target residual cancer cells.
Targeted therapy
This treatment targets specific genetic mutations or cellular weaknesses in cancer cells. Your doctor may test your tumor to identify the most effective targeted drugs for your cancer.
Hormone therapy
Hormone therapy blocks estrogen, which some ovarian cancer cells need to grow. It’s mainly used for slow-growing cancers or recurrent cases.
Immunotherapy
Immunotherapy helps the immune system recognize and attack cancer cells. It may be recommended for specific ovarian cancer types that respond to immune-based treatment.
Supportive (palliative) care
Palliative care provides symptom relief and emotional support for people with serious illnesses. It can be combined with active treatment to enhance quality of life and, in some cases, improve survival.
A palliative care team—comprising doctors, nurses, and specialists—works alongside your primary care team to manage pain, fatigue, and other symptoms, ensuring comfort throughout the treatment process.
Advertisement