Overview
Diagnosis
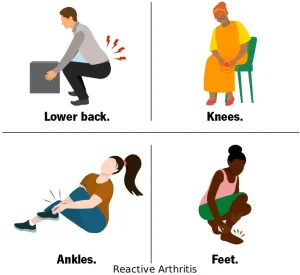
During the physical exam, your doctor may check your joints for swelling, warmth and tenderness. The range of motion in your spine and affected joints is often tested to assess how inflammation is affecting movement. Your doctor may also examine your eyes for inflammation and your skin for rashes, which can be associated with reactive arthritis.
Blood tests may be done to look for signs of infection, inflammation, certain antibodies linked to other forms of arthritis and a genetic marker connected to reactive arthritis. A sample of joint fluid may also be collected using a needle. This fluid is tested for white blood cell count, which can indicate inflammation or infection; the presence of bacteria, which may suggest septic arthritis; and uric acid crystals, which may point to gout. Imaging tests such as X-rays of the low back, pelvis and joints can help identify signs of reactive arthritis and rule out other conditions.
Treatment
Treatment focuses on managing symptoms and addressing any persistent infection. If reactive arthritis is linked to a bacterial infection, antibiotics may be prescribed depending on the specific bacteria involved. To ease symptoms, several medications may be used:
-
Nonsteroidal anti-inflammatory drugs, such as indomethacin, can help relieve pain and inflammation.
-
Steroid injections may reduce inflammation in affected joints, while steroid eye drops or creams may be used for eye and skin symptoms.
-
Certain medications used for rheumatoid arthritis, including sulfasalazine, methotrexate or etanercept, may provide relief for some people.
Physical therapy can support recovery by offering strengthening exercises to improve muscle support around affected joints and range-of-motion exercises to increase flexibility and reduce stiffness.
Advertisement