Overview
Diagnosis
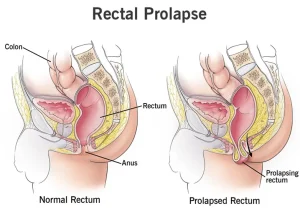
Sometimes rectal prolapse can be difficult to distinguish from hemorrhoids. To confirm rectal prolapse and rule out other conditions affecting the rectal area, several tests may be recommended. A digital rectal exam is often the first step. During this exam, a healthcare professional inserts a gloved and lubricated finger into the rectum to check the strength of the anal sphincter muscles and identify any structural issues. You may be asked to bear down so the clinician can look for signs of prolapse.
Anal manometry may be used to measure how well the rectum and anal sphincter are working. This test involves inserting a thin, flexible tube into the anus and rectum. A small balloon at the tip can be inflated to help measure muscle tightness and function.
A colonoscopy might be done to rule out conditions such as hemorrhoids, colon polyps or colon cancer. In this procedure, a flexible tube is inserted into the rectum to examine the entire colon.
Another helpful imaging test is defecography. This test involves using a dye during an X-ray or MRI scan. It helps show changes in the structure of the lower digestive tract and provides information on how the rectal muscles function during bowel movements.
These tests help your healthcare team make an accurate diagnosis and determine the best treatment approach for your condition.
Treatment
Treatment for rectal prolapse often involves surgery to correct the prolapse and restore normal function. Management of constipation is also important and may include stool softeners, suppositories or other medications to make bowel movements easier and reduce strain.
There are several surgical options for rectal prolapse. The choice of procedure depends on factors such as your age, overall health and bowel function. Your healthcare professional will discuss the most suitable approach for your situation. Some procedures are performed through the abdomen, while others are done through the rectum. The goal of treatment is to repair the prolapse, improve symptoms and prevent future problems.
Advertisement