Overview
Diagnosis
A diagnosis of rumination syndrome begins with a review of symptoms and a detailed medical history. This initial evaluation, along with observing the pattern of regurgitation, is often enough for a healthcare professional to identify the condition. In some cases, additional tests such as high-resolution esophageal manometry and impedance measurement may be used. These tests help detect increased abdominal pressure and show irregular function that can guide behavioral therapy.
Other tests may be done to rule out other causes of symptoms, including:
-
Upper endoscopy to closely examine the esophagus, stomach and upper small intestine, and to remove a biopsy if needed
-
Gastric emptying studies to measure how long it takes food to move through the stomach, small intestine and colon
Treatment
Treatment for rumination syndrome begins after other conditions are ruled out and varies based on age and cognitive ability.
Behavior therapy
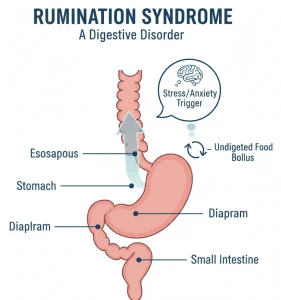
Habit-reversal behavior therapy is commonly used for people without developmental disabilities. This approach teaches awareness of rumination and uses diaphragmatic breathing to stop abdominal contractions that cause regurgitation. Biofeedback may support this process by providing visual guidance to help learn and apply proper breathing techniques.
For infants, treatment focuses on adjusting the environment and working with parents or caregivers to change behaviors that may contribute to symptoms.
Medicine
Some individuals may benefit from medicines that relax the stomach after meals. If repeated rumination causes irritation or damage to the esophagus, proton pump inhibitors such as esomeprazole or omeprazole may be recommended. These medicines protect the esophageal lining until behavior therapy reduces the frequency and severity of regurgitation.
Advertisement