Overview
Diagnosis
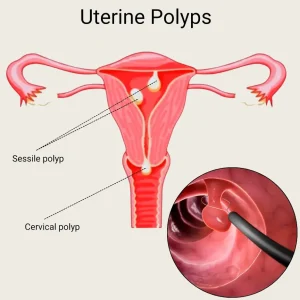
Uterine polyps are growths on the inner lining of the uterus (endometrium). Diagnosis typically involves imaging and tissue sampling to confirm the presence of polyps and rule out cancerous changes.
Common diagnostic tests include:
-
Transvaginal ultrasound: A slender, wandlike device (transducer) is placed in the vagina. Sound waves create images of the uterus, ovaries, and fallopian tubes. Polyps or areas of thickened endometrial tissue may be visible.
-
Hysterosonography (sonohysterography): Saline is injected into the uterus through a thin tube inserted via the vagina and cervix. The expanded uterus provides clearer ultrasound images of the uterine cavity.
-
Hysteroscopy: A thin, flexible, lighted telescope (hysteroscope) is inserted through the vagina and cervix into the uterus, allowing direct visualization of the uterine lining.
-
Endometrial biopsy: A suction catheter collects a small tissue sample from the uterus. This helps confirm the presence of polyps and rule out precancerous changes or uterine cancer.
Most uterine polyps are benign. However, tissue analysis is important because some polyps may contain precancerous changes or cancer cells.
Treatment
Treatment for uterine polyps depends on the size, symptoms, and risk of cancer.
-
Watchful waiting: Small, asymptomatic polyps may resolve on their own. Treatment may not be necessary for individuals not at risk of uterine cancer.
-
Medication: Hormonal medications, including progestins and gonadotropin-releasing hormone agonists, may help reduce symptoms temporarily. Symptoms often return after stopping the medication.
-
Surgical removal: Polyps can be removed during hysteroscopy using instruments inserted through the hysteroscope. Removed polyps are typically sent for lab analysis to check for cancer cells.
If a polyp contains cancerous cells, your healthcare provider will discuss further evaluation and treatment options.
-
Recurrence: Rarely, polyps may recur after removal, which may require additional treatment.
Advertisement